The state provides about $1.6 billion in funding to the Department of State Hospitals (DSH) to provide inpatient treatment to mental health patients in the eight DSH facilities. This includes funding for both clinical and nonclinical staff, as well as non–staff costs (such as food and clothing). In determining how much funding to request for the upcoming fiscal year, DSH uses the amount of funding it received in the state budget for the current year as a base budget or starting point. The department then requests adjustments to the base budget to account for projected increases or decreases in the patient population during the budget year.
DSH’s Budgeting Process Has Several Shortcomings. Based on our review, we find that the current DSH budgeting process has several shortcomings. Specifically, we find that (1) the department has a large amount of funded beds that are not used; (2) the level of staff needed to operate DSH facilities is unclear; (3) the budgeting methodology used by the department creates poor incentives for it to operate efficiently; and (4) other state departments have more transparent, updated, and efficient budgeting processes than DSH.
Redesigning DSH’s Budgeting Process. In view of the above findings, we make several recommendations to improve the DSH budgeting process. First, we recommend the Legislature require the department to establish or update several key components used to develop its budget to ensure that they are accurate and adequate. Second, we recommend that the Legislature direct DSH to use the updated information to develop its budget and staffing requests based on expected changes in the number and acuity (or level of care) of its patient population, as well as make adjustments to its budget if the actual population differs from its projections. Given the resources and time necessary to implement these recommendations, we also recommend that the Legislature require DSH to provide additional justification for its budget requests during the development and implementation of the new budgeting process. In combination, we believe our recommendations will (1) ensure that DSH receives the appropriate amount of funding to account for changes in its patient population and the services it provides, (2) improve incentives for the department to operate efficiently, and (3) allow the Legislature to provide increased oversight of DSH’s budget and operations.
The DSH provides a variety of inpatient behavioral health services to more than 6,600 patients at five state hospitals and three prison–based psychiatric programs. In recent years, the number of patients referred to DSH for treatment has increased, and the patient population has grown about 14 percent since 2010–11. As part of the 2014–15 budget, the state provided additional funding to the department to accommodate this increase, including resources to activate nearly 250 additional beds. Despite the increased resources, the department had a patient waitlist of nearly 550 individuals as of January 2015. Maintaining such a long waitlist for DSH placement delays access to care for patients, as well as poses legal risks for the department. This is because if DSH fails to admit patients waiting for care within certain time frames, the department can be required to appear in court and potentially be held in contempt.
In recent years, concerns have been raised about DSH’s budgeting process, including some problems that contribute to the department’s increasing waitlist. For example, in our report The 2014–15 Budget: Analysis of the Health Budget, we noted that the department’s process for patient placement does not efficiently utilize bed space across the system and that there are large discrepancies between the number of beds the department is budgeted for and their actual patient population. In this report, we examine these and other problems with the DSH budget process. Specifically, we (1) provide an overview of how the department develops its annual budget requests, (2) highlight some shortcomings of that process and contrast those with best practices in other departments, and (3) recommend steps the Legislature can take to make DSH’s budget process more transparent and to incentivize the department to deliver care more cost–effectively.
In preparing this report, we spoke with state hospital administrators and behavioral health care providers in California and other states. We also spoke with other large state health care providers, including the federal court–appointed Receiver overseeing prison health care, the California Department of Corrections and Rehabilitation (CDCR), and the California Department of Public Health (CDPH). In addition, we visited various state hospitals and psychiatric programs operated by DSH. We also reviewed academic literature regarding inpatient behavioral health treatment and analyzed data from numerous sources, including DSH and similar departments in other states.
The DSH was established in 2012. Specifically, Chapter 29, Statutes of 2012 (AB 102, Committee on Budget), eliminated the Department of Mental Health (DMH) and transferred the responsibility for delivering inpatient behavioral health services to patients at state hospitals from DMH to DSH. The Governor’s budget includes a total of $1.7 billion for DSH, which is roughly the same level provided in the 2014–15 budget. The department currently treats 6,600 patients at its eight facilities. (Please see the box California’s State Hospital System for additional information regarding DSH’s facilities.) The average length of stay for DSH patients is less than one year.
California has five state hospitals and three psychiatric programs located on the grounds of the prisons operated by the California Department of Corrections and Rehabilitation.
Atascadero State Hospital. This facility, located on the Central Coast, houses a largely forensic population, including a large number of incompetent to stand trial patients and mentally disordered offenders. As of December 2014, it housed more than 1,000 patients.
Coalinga State Hospital. This facility is located in the city of Coalinga and is California’s newest state hospital. The hospital houses only forensic patients, most of whom are sexually violent predators. As of December 2014, it housed more than 1,100 patients.
Metropolitan State Hospital. Located in the city of Norwalk, this hospital’s population is approximately 65 percent forensic. Metropolitan State Hospital does not accept individuals who have a history of escape from a detention center, a charge or conviction of a sex crime, or a conviction of murder. As of December 2014, it housed about 700 patients.
Napa State Hospital. This facility is located in the city of Napa and has a mix of civil and forensic commitments. Napa State Hospital limits the number of forensic patients to 80 percent of the patient population. As of December 2014, it housed nearly 1,200 patients.
Patton State Hospital. This facility is located in San Bernardino County and primarily treats forensic patients. As of December 2014, it housed 1,500 patients.
Salinas Valley Psychiatric Program. This program is located on the grounds of Salinas Valley State Prison in Soledad and provides treatment to state prison inmates. As of December 2014, it had a population of more than 200 patients.
Stockton Psychiatric Program. This program is located on the grounds of the California Health Care Facility in Stockton and is the state’s newest psychiatric program. The program provides treatment to state prison inmates. As of December 2014, it had a population of about 400 patients.
Vacaville Psychiatric Program. This program is located on the grounds of the California Medical Facility in Vacaville and provides treatment to state prison inmates. As of December 2014, it had a population of about 350 patients.
Patients at the state hospitals receive 24–hour care (including therapy and medication) and fall into one of two categories: civil commitments or forensic commitments. Civil commitments are generally referred to the state hospitals for treatment by counties. This is because they have a mental illness that makes them a danger to themselves or others or makes them gravely disabled. Forensic commitments are typically committed by the courts and include state prison inmates referred by CDCR as well as individuals classified as incompetent to stand trial, not guilty by reason of insanity, mentally disordered offenders (individuals referred by the Board of Parole Hearings to DSH as a condition of state parole), or sexually violent predators. The forensic population of the state hospitals has been consistently high in the past decade, averaging roughly 90 percent of the state hospital population. Currently, 92 percent of state hospital patients are forensic commitments.
The vast majority (about 98 percent) of DSH’s budget is devoted to treating patients in the eight DSH facilities. Below, we discuss how DSH develops its annual budget requests to provide such treatment. Specifically, we describe how the department (1) uses the base budget as a starting point, (2) projects changes in its patient population, (3) adjusts staffing levels to account for such population changes, and (4) sometimes adjusts for non–staff costs. Figure 1 provides an overview of the department’s budgeting process.
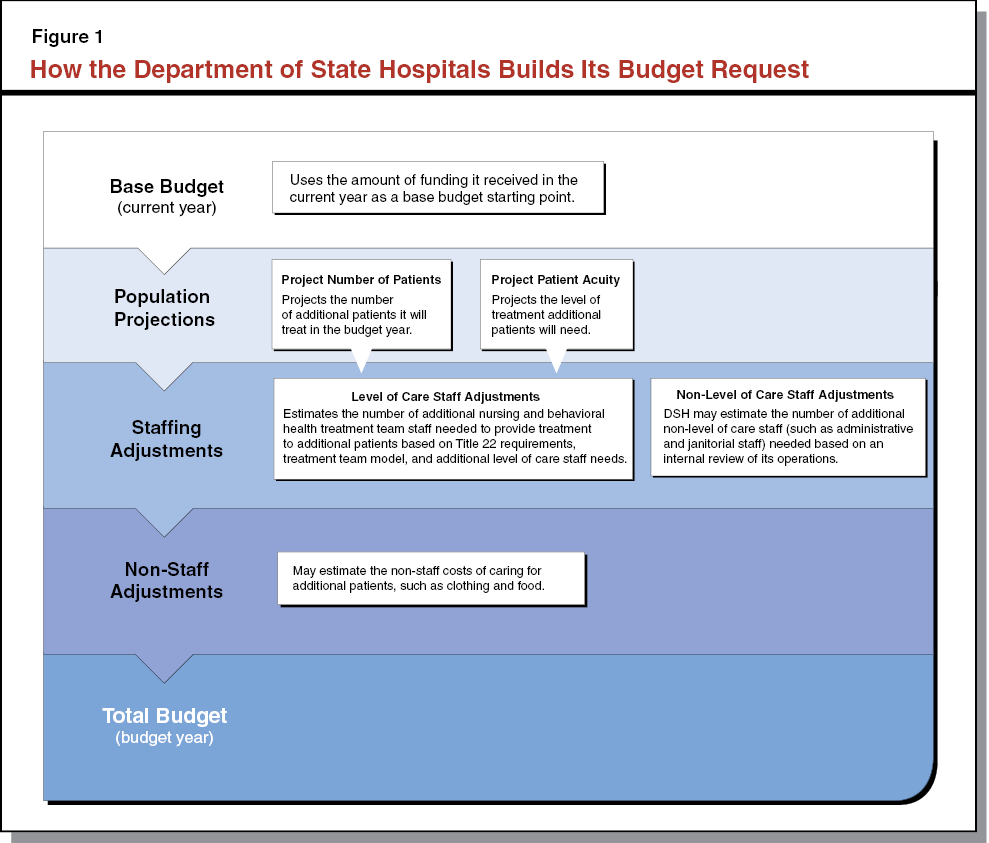
In determining how much funding to request for the upcoming fiscal year, the department uses the amount of funding it received in the state budget for the current year as a base budget or starting point. For example, the department’s budget for 2014–15 becomes the base budget for 2015–16. The base budget includes the total amount of funding to treat DSH patients, including non–staff and staff costs. The department then requests adjustments to the base budget to account for projected increases or decreases in the patient population during the budget year, as we describe below.
Projecting the Number of Patients. In developing its annual budget request, DSH projects the number of patients it will treat in the upcoming fiscal year—particularly in terms of changes relative to the current fiscal year. The main factors that inform the department’s projections are (1) the number of patients being treated in the current year and (2) the number of patients on its waitlist for treatment. Based on the expected change in the patient population, DSH then estimates how many beds it will need to treat those patients. If the department projects an increase in the population, as has been the case in recent years, it requests funding to activate enough new beds to accommodate the increase. We note, however, that the department may propose activating a smaller number of beds if it lacks the infrastructure or operational capacity to activate the full amount needed to accommodate the increase. After estimating the number of additional beds it needs to activate relative to the current year, the department’s next step is estimating the acuity level of the patients who will fill those beds.
Projecting Patient Acuity. Patients treated in DSH facilities require varying levels of treatment based on the severity of their diagnoses and the treatment plan that their treatment teams develop. Based on these assessments, the department classifies patients as needing one of three levels of care (commonly referred to as acuity levels).
- Intermediate Care Facility, which provides inpatient skilled nursing services to patients who do not require continuous nursing care.
- Acute, which provides 24–hour inpatient care services, including medical, behavioral health, and pharmaceutical services.
- Skilled Nursing Facility, which provides long–term skilled nursing care, including 24–hour inpatient treatment and a variety of physical and behavioral health services.
These acuity levels are associated with the licensing standards specified in Title 22 of the California Code of Regulations and specific clinical staffing levels developed by DSH, which we discuss in more detail below. Because the acuity levels of patients affect the number and cost of clinical staff necessary to provide care, the department must estimate the acuity level of any additional patients for the budget year. The estimate is developed in consultation with clinical executives and facility staff and is generally based on the acuity profile of the current patient population.
Based on the projected number of additional patients that will need to be treated in the coming fiscal year, as well as the estimated acuity profile of those patients, the department requests additional staff. If DSH estimates a reduction in its patient population, which has not happened in recent years, a similar methodology could be used to make staffing reductions.
Level of Care Staff Adjustments. Level of care staff provide treatment services to DSH patients, and include nursing staff and behavioral health treatment team staff. When DSH requests adjustments to its level of care staffing levels based on the expected change in the patient population, it considers the following three factors.
- Title 22 Requirements. Title 22 of the California Code of Regulations sets the standards for operating an acute psychiatric hospital. Specifically, Title 22 requires hospitals to be licensed by CDPH and sets minimum requirements for staffing and facilities. In particular, it requires a certain minimum number of nursing staff based on patient acuity and associated treatment needs for different nursing shifts (meaning morning, afternoon, or overnight), as shown in Figure 2. Title 22 nursing staff have many responsibilities, including patient observation, medication distribution, and patient escorting.
- Treatment Teams. In addition to the nursing staff required by Title 22, DSH also uses a behavioral health treatment team model. Under this model, clinicians work together to provide individual and group treatment to a set number of patients. Each treatment team includes five providers—a psychiatrist, psychologist, social worker, rehabilitation therapist, and a registered nurse. Treatment team nursing staff are distinct from Title 22 nursing staff in that they are responsible for developing treatment plans and participating in treatment team meetings. They have an assigned group of patients, rather than being assigned to morning, afternoon, or overnight nursing shifts. The number of patients assigned to each treatment team is determined by patient acuity, as detailed in Figure 3.
- Additional Level of Care Staff. According to DSH, the staffing ratios described above do not account for certain services the department currently provides to patients. For example, the department indicates that the ratios do not account for an increase in recent years in the number of episodes where patients experience a severe crisis that requires one–to–one monitoring. As we discuss later in this report, the department has identified other workload that is also not reflected in the staffing ratios. To accommodate this workload, the department often augments its staffing requests with additional level of care staff beyond the Title 22 and treatment team staffing ratios. However, because these augmentations are not based on the department’s staffing model, it is difficult for the Legislature to assess the basis for these augmentations and whether they are appropriate.
Figure 2
Title 22 Staffing Requirementsa
|
Nursing Shift
|
Patient Acuity
|
|
Intermediate Care Facility
|
Acute
|
Skilled Nursing Facility
|
|
Morning
|
1:8
|
1:6
|
1:6
|
|
Afternoon
|
1:8
|
1:6
|
1:6
|
|
Overnight
|
1:16
|
1:12
|
1:12
|
Non–Level of Care Staff Adjustments. In addition to level of care staff, DSH also requires a variety of other staff to ensure its effective operation. These staff include nonbehavioral health clinicians, such as dieticians, medical doctors, administrative staff, janitors, firefighters, and hospital police. The number of non–level of care staff assigned to a particular facility is not necessarily directly related to the number of patients at the facility, and may be influenced by the design or age of the facility. As a result, non–level of care staff is not ratio–driven and the level of such staff at each facility varies. Currently, DSH determines the number of non–level of care staff at a facility based on internal assessments of its operations and needs. Headquarters may consult with specific facilities to determine whether changes to the patient population, services provided, or facility design requires an adjustment to the number or type of non–level of care staff at the facility. For example, the department could determine that activating a new patient treatment area results in a need for additional hospital police to monitor that area. Based on the department’s internal review, requests for adjustment to the number of non–level of care staff are sometimes included in population budget adjustments.
Figure 3
Treatment Team Staffing Ratiosa
|
Acuity Level
|
Staffing Ratio
|
|
Intermediate care facility
|
1:35
|
|
Acute
|
1:15
|
|
Skilled nursing facility
|
1:15
|
While DSH’s annual budget requests are typically limited to the staffing related adjustments described above, the department sometimes also requests adjustments for non–staff costs. These costs can include clothing, food, and facility costs. Generally, if the patient population increases, the department is required to absorb these costs within its existing base budget. However, that is not always possible. For example, if the department opens a new facility or experiences a large increase in the patient population compared to the previous year, the department could decide to request augmentations to its non–staff costs.
In order for DSH to ensure that its patients receive treatment in a timely, cost–effective manner, it is important that the department maintain efficient budgeting and bed management practices. These practices must also be transparent so that the Legislature has the information necessary to provide effective oversight. However, based on our review, we find that the DSH budgeting process has several shortcomings. Specifically, we find that (1) the department has a large amount of funded beds that are not used; (2) the level of staff needed to operate DSH facilities is not clear; (3) the budgeting methodology used by the department creates poor incentives for the department to operate efficiently; and (4) other state departments have more transparent, updated, and efficient budgeting processes than DSH. Figure 4 provides a summary of our major findings, which we discuss in further detail below.
Figure 4
DSH Budgeting Methodology Has Several Shortcomings
- Bed Vacancy Rate Has Been High in Recent Years
- Department Staffing Needs Are Unclear
- Level of care staffing model does not account for certain workload.
- Actual staffing exceeds Title 22 requirements and treatment team staffing model.
- Independent audits identified concerns with level of care staffing.
- Staffing needs have not been independently reviewed.
- DSH Budgeting Methodology Creates Poor Incentive Structure
- Budget process creates fiscal disincentive for DSH to fill vacant beds.
- Facilities have incentive to overestimate patient acuity.
- Other State Departments Have More Effective Budgeting Practices
|
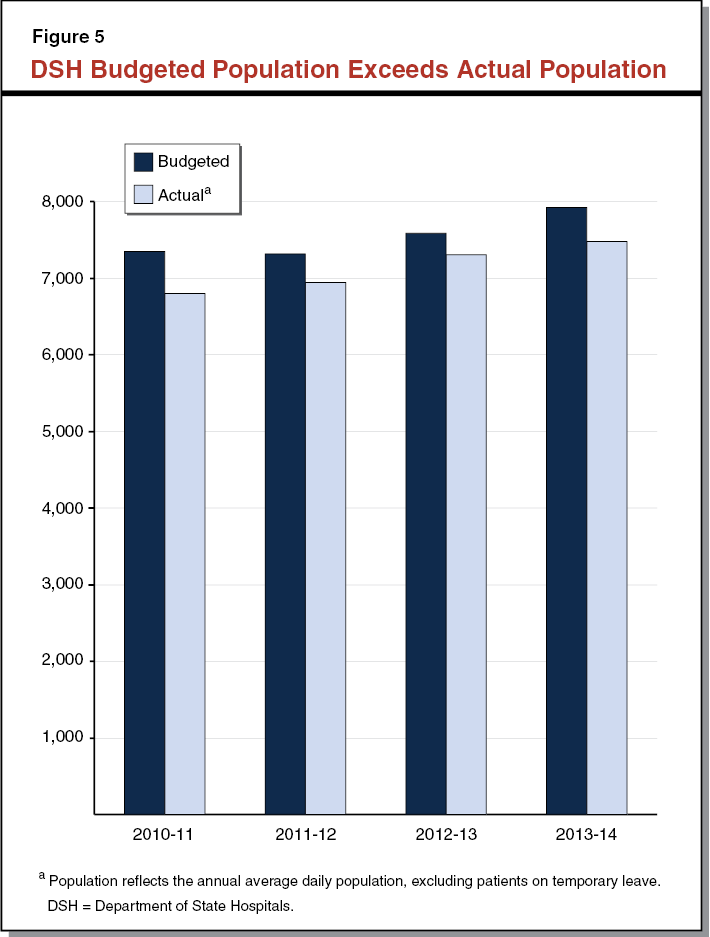
The number of patients that DSH actually treats relative to the number of patients it is funded to treat is known as the bed vacancy rate. As shown in Figure 5, DSH has consistently maintained several hundred vacant beds in recent years even through the department received funding to activate them. As of December 2014, DSH had 588 vacant beds, which is about 8 percent of their total budgeted capacity. This unutilized capacity comes at a high cost to the state, as each bed costs an average of almost $230,000 annually. Moreover, keeping funded beds vacant contributes to the department’s waitlist and delays access to care for patients. This is because beds that are vacant could otherwise be used to treat patients who are on the waitlist.
There are a variety of reasons why beds remain vacant even though the department received funding to fill them. Some of these reasons relate to how hospital facilities operate and are largely unavoidable. For example, about one–third of the department’s vacant beds are reserved for patients who are expected to return to the facility, such as those patients out for court or medical appointments. These patients are generally only away from the facility for short periods of time. Since the patients have not been discharged, they are still the responsibility of the department.
Currently, it is difficult to determine what factors account for the remaining two–thirds of the bed vacancies because DSH does not maintain the data necessary to conduct such an analysis. (We note that the department is in the beginning stages of collecting such data.) However, based on our review of the department’s budget, certain flaws in the department’s budgeting process could be contributing to the number of vacant beds. As discussed in detail below, the DSH budgeting process does not include appropriate fiscal incentives for the department to fill its vacant beds. In addition, according to the department, its staffing models have not been recently updated to reflect workload changes—creating pressure to redirect resources that would otherwise be used to fill the vacant beds.
We have identified several areas of concern with DSH’s current staffing. First, the department’s approach for determining its staffing levels has not been recently updated and thus may not account for certain workload. Second, our analysis indicates that there are significantly more level of care staff working for the hospitals than the department’s staffing ratios would suggest are necessary. Third, independent audits of DSH in recent years have raised questions regarding the appropriateness of the department’s staffing levels. Finally, despite these issues, the department’s staffing levels have not been recently independently reviewed.
Level of Care Staffing Model Does Not Account for Certain Workload. The DSH provides an array of treatment services to patients using a range of clinical staff. Since the department last revisited its level of care staffing levels in 2012, the type of services and the responsibilities of needed staff have evolved. However, according to DSH, the department’s clinical staffing model has not been adjusted to account for such changes. As discussed earlier in the report, the department typically redirects staff or requests additional level of care staff to support the services not accounted for in the staffing model. For example, the model does not account for a recent change in how the department provides group treatment. Historically, DSH patients have received treatment exclusively from treatment teams assigned to their housing unit (or nearby units). In recent years, however, the department started providing group therapy outside of a patient’s housing unit. This allows the department to provide group treatment to patients with similar diagnoses or treatment needs, regardless of whether they live in the same housing unit. Level of care staff manage these group treatment sessions, and may also be required to escort patients from their housing units to the group treatment areas. According to DSH, the current level of care staffing ratios do not account for such off–unit services and escorting needs.
The level of care staffing also does not account for changes in the needs of the patient population. According to the department, the patient population has become more difficult and violent in recent years, which has increased the need for more intensive care. For example, patients experiencing a mental health crisis or feelings of suicidality require one–to–one staffing. This often requires the department to shift staff from treating other patients to provide enhanced services to these particular patients. As a result, the department may not be consistently providing all the services that patients require.
The changes to level of care workload without corresponding changes to the staffing model could be contributing to the department’s high bed vacancy rate in recent years. Specifically, it is possible that the department is redirecting staff from beds for which it is funded to operate in order to provide the level of group treatment and one–to–one monitoring described above, which would then result in the beds being vacant. While the additional services and activities may be warranted, the redirection of staff for this purpose raises a few concerns. In particular, the redirection of staff could be limiting the department’s ability to reduce its waitlist. In addition, while these new services may be consistent with legislative priorities, the Legislature has not approved funding for this specific purpose. As such, the practice of redirecting funding in this manner undermines the Legislature’s ability to ensure that its priorities are being met.
Actual Staffing Exceeds Title 22 Requirements and Treatment Team Staffing Model. To account for the shortcomings in the model discussed above, in recent years DSH has requested, and the Legislature has approved, augmentations to its staffing. Because of these augmentations, DSH has consistently maintained higher staffing levels than would be expected based on Title 22 standards and the treatment team staffing model. In order to assess this difference, we compared the expected number of statewide nursing and treatment team staff, based on the department’s actual patient population, to its actual staffing levels in 2013–14. We found that the department employed about 35 percent more staff than required under Title 22 and DSH’s own staffing model. This equates to nearly 2,000 nurses and more than 200 psychiatrists, psychologists, rehabilitation therapists, and social workers in excess of the expected staffing level. We note that in recent years the gap between the level of care staffing and actual staffing levels has declined. However, the fact that such a significant discrepancy persists provides further evidence that the department’s level of care staffing ratios are no longer useful. Additionally, while some deviation from the staffing ratios may be needed to cover additional workload, the large size of the gap raises questions about whether the augmentations are necessary.
Independent Audits Identified Concerns With Level of Care Staffing. In recent years, the Office of State Audits and Evaluation (OSAE) at the Department of Finance and the Coleman Special Master (who provides court oversight for state prison inmates who are committed to DSH facilities) have raised concerns with DSH’s staffing. Their findings, which we summarize below, provide additional evidence that the department’s staffing methodology is outdated.
- Staffing Does Not Result in Optimal Patient Outcomes. In May 2014, the Coleman Special Master released a report that raised several concerns with the quality of care provided in DSH facilities. The report noted that the department was providing far less group therapy than it should. According to the report, care was widely inconsistent, often nontherapeutic, and did not include certain types of treatment, even when patients clearly required such treatment.
- Clinical Staff May Be Performing Tasks That Could Be Performed by Lower Skill Classifications. A 2008 OSAE report cited concerns from hospital staff that clinical staff were performing administrative functions that could be performed by non–level of care staff. The audit noted that shifting administrative workload to nonclinical staff could result in costs savings for the department.
- Staff Savings Are Redirected for Operating Expenditures. The 2008 OSAE report noted that DSH had a practice of redirecting savings from its staffing budget to cover deficiencies in its operations budget.
Staffing Needs Have Not Been Independently Reviewed. Until 2013, DSH was under a consent decree pursuant to the federal Civil Rights for Institutionalized Persons Act (CRIPA), which is designed to protect individuals in public institutions such as mental hospitals. The terms of the consent decree limited the state’s ability to adjust DSH’s level of care staffing. Given that the department is no longer under court oversight, it is now in a position to reassess whether its existing staffing levels are appropriate. While the department performed an internal review of level of care staffing upon exiting CRIPA court oversight, that review was limited and culminated in only a slight modification to its treatment team staffing ratios. Recently, DSH initiated an additional internal review of its nursing staffing levels and responsibilities. However, the department has not yet undertaken a comprehensive review of its other clinical staffing levels. Moreover, reviews performed in the past, and the current nursing staffing review, have not been performed by an independent agency. As we discuss below, this is in contrast to independent staffing reviews completed by the Receiver in recent years.
There is also evidence that the department’s non–level of care staff may not be adequate. In May 2012, the department reported that non–level of care staffing in the hospitals may be insufficient. Since that time, however, the DSH has not comprehensively reviewed the non–level of care staffing at its facilities to ensure that staffing levels are adequate to achieve the department’s mission. In addition, the department has not reviewed the responsibilities of these staff to ensure that staff are being efficiently used. Although the department hopes to do an internal review of its non–level of care staffing in the near future, it does not have plans for an independent review.
The current budget process provides little fiscal incentive for the department and individual DSH facilities to fully utilize their budgeted capacity and accurately project patient acuity. As noted above, failure to operate efficiently means patients may wait longer for treatment or treatment may be more costly than necessary. As we discuss below, the current budget process does not incentivize such efficient operation.
Budget Process Creates Fiscal Disincentive for DSH to Fill Vacant Beds. Unlike other similar state departments, DSH’s budget is not typically adjusted to reflect its actual patient population, including the number of vacant beds. In 2013–14, the department had an average bed vacancy of nearly 450 beds. At an annual average bed cost of $230,000, the total cost of these vacant beds was more than $100 million. However, at the end of 2013–14, the department only reverted $28 million to the General Fund. This is despite the fact that most of the funding tied to the unutilized capacity (such as for staff, clothing, and food costs) was not needed for its intended purpose and could have been reverted to the General Fund.
Because the department’s budget is not typically adjusted based on the actual population, it has no fiscal incentive to ensure that all its beds are filled. This incentive to maintain vacant beds is further compounded by workload for which the department is not specifically funded. As we note above, the department has expanded the services it provides and has experienced an increase in workload associated with higher patient care needs. However, the department has not been specifically funded for those responsibilities. This creates an incentive for the department to maintain vacant beds so that it can redirect staff associated with the vacant beds to support these unfunded services.
Facilities Have Incentive to Overestimate Patient Acuity. According to DSH, facilities receive additional funding and staff if they expect to have an increase in high acuity patients. Since the additional funding is not adjusted for actual patient acuity, there is an incentive for facilities to overestimate the needs of their patients. If a facility projects that incoming patients will have acute (as opposed to intermediate) care needs, it will receive additional staff and funding to provide such care. On the other hand, if the patient population is actually more acute than expected, DSH’s budget and staffing is not adjusted to reflect the costs of providing the higher level of care. If the actual patient population is not as acute as projected, though, the department is not required to revert any funding. As such, an overestimation of patient acuity can result in the department spending more than is necessary to treat its patients.
The incentive for facilities to overestimate patient acuity is strengthened by the fact that the current acuity model may not accurately reflect patients’ needs. According to the department, there has been an increase in the number of violent incidents and some patients require more care and monitoring than is possible under any of the current acuity designations. For example, Chapter 718, Statutes of 2014 (AB 1340, Achadjian), established a program in DSH facilities to provide enhanced treatment for the most violent patients. The enhanced treatment unit (ETU) requires a staff–to–patient ratio of 1:5, which is higher than the ratios required for any of the existing acuity levels. However, the ETU staffing requirements are currently not part of the department’s acuity model and projection process. If patients have higher care needs—such as those found in the ETUs—than are accounted for under the current acuity model, facilities may need additional staff beyond what is estimated by the model. Since those staff are not accounted for with the current acuity model, there is an incentive to assume that new patients will have a high level of acuity in order to receive additional funding and additional staff that could then be redirected to provide more intensive services to those patients that actually have high needs.
Although the DSH budgeting process creates poor incentives such as those described above, it is possible to establish a budgeting process that better incentivizes efficiency. As we discuss below, other state departments take a different approach to budgeting, which creates more transparency and appropriate incentives to accurately budget and staff facilities.
While DSH provides unique services, it does have some similarities to other state departments, particularly CDCR and the Receiver’s office. For example, these two agencies face similar issues (such as balancing patient needs with security concerns) as well as require similar staffing mixes, including level of care and non–level of care staff. However, CDCR and the Receiver have a different approach than DSH in terms of budgeting and allocating staff positions. Some of the major differences between their process and the DSH process include:
- Independent Staffing Analysis. Like DSH, the Receiver also had a staffing plan that until recently did not account for all the workload and requirements the department faced. Because of the discrepancies between the Receiver’s staffing plan and actual workload, the Receiver’s office recently contracted for independent analyses of its staffing. The analyses included a review of staff responsibilities, patient acuity, the volume and variety of services that must be provided, facility–specific factors (such as proximity to community hospitals), and other related factors. These analyses developed new clinical staffing ratios and provided comparisons to the staffing ratios of other similar organizations.
- Ratio–Driven Level of Care Staffing. Based on the above independent staffing analyses, the Receiver now uses a ratio–driven staffing model. Under the model, the Receiver estimates inmates’ medical acuity based on the projected inmate population for the budget year. The Receiver then applies these estimates to the staffing ratios developed by the staffing analyses. Under this model, statewide staffing levels are determined by a formula that accounts for all clinical workload—meaning separate staffing augmentations are not necessary. Once statewide staffing levels are determined, the Receiver determines the appropriate allocation of staff positions to each prison.
- Non–Level of Care Staffing. In response to the Farrell v. Brown court case, the CDCR Division of Juvenile Justice (DJJ) contracted with a consultant to develop a new staffing model, which includes both facility–specific and population–driven non–level of care staffing. For example, each DJJ facility receives one groundskeeper position for every 30 acres. These staff are adjusted annually based on changes to the population or facilities. For example, if a facility closes, the groundskeeper position would be eliminated. In contrast, DSH makes adjustments to non–level of care staff on occasion, but does not do so in a regular and standardized manner.
- Adjustment for Actual Population. The Receiver’s office adjusts its staffing levels for the actual patient population. Like DSH, the Receiver’s office must project its future population. However, unlike DSH, the Receiver’s office (1) biannually reviews any differences between its estimated population and acuity and the actual population and acuity and (2) adjusts its staffing and budget based on those reviews. For example, if the inmate population is higher than expected, the Receiver may request additional funding. On the other hand, if the population is lower than expected, the corresponding amount of savings may revert to the General Fund. We note that CDCR has a similar process to the Receiver for adjusting its budget based on actual population levels.
- Adjustment for Acuity Level. The Receiver has an acuity classification model similar to DSH, with funding and staff tied to patient acuity. At the beginning of each calendar year, the Receiver projects the number of inmates who will require each level of care. Every six months, the Receiver reviews its projections and adjusts its budget based on that review. If patient acuity was underestimated, the Receiver may request additional funding to cover the higher workload. If patient acuity is overestimated, the corresponding amount of savings may revert to the General Fund.
- Validation of Acuity Designations. The Receiver also uses a quality control process to ensure that inmates are assigned to the correct level of care, in order to avoid, for example, classifying an inmate as needing a higher level of care than they actually require. The Receiver’s quality control process requires at least two clinical staff to review whether an inmate’s acuity level has been appropriately assessed. If the reviewers find that patients are inappropriately placed, then the department may refine or clarify acuity criteria, or provide additional staff training. This ensures that the process by which inmates are assigned to acuity levels is accurate and consistent.
In this report, we reviewed the process that DSH currently uses to develop the population–driven portion of its budget and identified several concerns with the process. Based on our findings, we make several recommendations below to improve the DSH budgeting process in order to ensure that the department provides inpatient behavioral health services in a timely, cost–effective manner. Specifically, we recommend the Legislature (1) require the department to establish or update several key components used to develop its budget to ensure that they are accurate and adequate and (2) direct DSH to use the updated information to develop its budget and staffing requests based on expected changes in the number and acuity profile of its patient population. Given the resources and time necessary to implement these recommendations, we also recommend that the Legislature require DSH to provide additional justification for its budget requests during the development and implementation of the new budgeting process. Figure 6 summarizes our recommendations, which we discuss in greater detail below.
Figure 6
LAO Recommendations for Redesigning DSH’s Budget Process
- Revise Components of DSH’s Budget Process
- Validate patient acuity model.
- Update staffing methodology.
- Establish standardized per patient non–staff cost.
- Make Adjustments Based on Actual Patient Population and Acuity Levels
- In Short Run, Require DSH to Provide Additional Information to Justify Budget Requests
|
Based on our findings, we recommend several changes to the DSH budgeting and staffing process. For that process to be effective, however, the information that is used to build the staffing and population adjustments must be up–to–date. Specifically, we recommend (1) validating the patient acuity model, (2) updating the department’s staffing methodology, and (3) establishing a standardized non–staff cost per patient.
As discussed earlier, DSH facilities currently have an incentive to overestimate patient acuity and the current acuity model may not capture the higher care needs of a forensic patient population. We also note that the department has not recently updated its acuity model. Based on those findings, we recommend that the Legislature require the department to (1) contract for an independent analysis of its patient acuity designations and (2) establish an ongoing acuity designation process.
Independent Analysis of Acuity Designations. The independent analysis should include a review of the appropriateness of the current acuity levels and recommendations for any revisions or additions to the current model. Based on the results of this analysis, the department should adjust its acuity model to ensure that it is up–to–date and accurately reflects the treatment needs of its patients. We expect that such a review could be achieved with minimal cost by leveraging existing resources and contracts. The department is currently negotiating a contract to inventory its capacity of beds by acuity and use. The assessment of the appropriateness of the acuity model could be added to the scope of that related project.
Ongoing Acuity Review Process. After DSH updates its acuity model based on the findings of an independent analysis, the department should establish an ongoing process to control for the quality of how it designates patient acuity. In order to facilitate this process, we recommend that the Legislature adopt language similar to the Title 22 requirements for general acute care hospitals, which require hospitals to annually review the reliability of their patient acuity designation model. This review is performed by clinical staff, at least half of whom must provide direct care. There are two major benefits to this quality control process. First, it would ensure that patients are being appropriately assigned to acuity levels and that the process to assign patients is consistent statewide. Second, it would reduce the ability of facilities to systematically overestimate patient acuity.
We recommend that the Legislature require DSH to make several changes to the process by which it determines the appropriate level of staffing for its facilities, including updating staffing models for both level of care and non–level of care staffing.
Update Level of Care Staffing. As discussed earlier, DSH’s level of care staffing models have not been updated to account for recent operational changes and independent audits have raised questions about the appropriateness of the department’s staffing methodology. Accordingly, we recommend that the Legislature require DSH to contract with an independent consultant for a comprehensive clinical staffing analysis. Such an analysis should include: (1) an evaluation of the department’s clinical staffing, including treatment team and nursing staff; (2) an assessment of the appropriate number and type of clinical staff necessary to provide treatment for patients assigned to each acuity level; (3) an assessment of whether staff are assigned appropriate responsibilities, or whether some tasks could be assigned to nonclinical staff or less costly clinical staff; and (4) recommendations to ensure the department is utilizing its staff as efficiently and effectively as possible. We estimate that such an analysis would likely cost less than $100,000.
We further recommend the Legislature require DSH to use the findings of the above analysis to implement a new, ratio–driven treatment team staffing model similar to the one used by the Receiver. Under this approach, the department would set staffing ratios as determined by the independent analysis and Title 22 requirements. As we discuss below, the department would project its patient population for the coming fiscal year and then apply the staffing ratios to determine a statewide staffing level. The DSH would then be able to allocate those staff positions to each facility based on its assessment of each facility’s needs. Our proposal would streamline the population adjustment process and ensure transparency about how DSH determines the level of staff necessary to provide care to the patient population.
Update Non–Level of Care Staffing. In addition to revising the level of care staffing, we also recommend the Legislature require DSH to contract for an independent review of its non–level of care staffing. Because this type of staffing is frequently facility–specific and includes a wide variety of classifications, we recommend the analysis be performed separately from the above level of care staffing analysis. The non–level of care staffing analysis should review the number and type of staff assigned to each facility, as well as an assessment of their responsibilities. This analysis should also ensure that all staffing levels are consistent and up–to–date, and include recommendations to ensure efficient and effective delivery of treatment. It should also result in staffing ratios similar to those used by DJJ, including ratios based on facility factors and patient population. This analysis, which would likely cost less than $100,000, could be included with the level of care staffing analysis contract. Under our proposal, the Legislature would be able to ensure that non–level of care staffing is appropriate and accounts for current department workload.
We recommend that the Legislature require DSH to use a per patient, non–staff cost estimate, similar to the estimates used by CDCR and the Receiver. The estimate should include all variable non–staff costs associated with caring for an individual patient (such as clothing and food), but exclude fixed costs associated with operating all DSH facilities (such as facilities maintenance). The Legislature could use this cost estimate to adjust DSH’s budget to account for changes in the patient population, such as slower than projected growth in the patient population, as we discuss in more detail below.
Given the lack of appropriate incentives for DSH to utilize its full capacity and appropriately assess patient acuity, we recommend that the Legislature require the department to submit budget requests based on the number and acuity profile of the patients it actually serves, similar to the budgeting methodology used for CDCR and the Receiver. Our proposed process for adjusting DSH’s budget would resemble its existing process in a couple respects. As with the current budget process, the department would submit as part of the Governor’s January budget an estimate of the patient population by acuity level for the upcoming fiscal year. These estimates would be the basis for the department’s budget requests. Also, like the current process, the department would make any necessary adjustments to its budget request based on updated population information as part of the Governor’s May Revision.
Current–Year Funding Adjustments. However, our proposed process would differ from the existing process in a couple important respects. First, under our proposal, DSH would biannually provide updated information comparing its current–year patient population by acuity level (based on actual year–to–date data) to the levels assumed in the enacted budget for the current year. Second, the department’s proposed budget and staffing adjustments would be directly and explicitly based on the updated cost estimates we described above.
For example, when the department submits its budget request as part of the Governor’s January budget for 2017–18, the department would include an updated estimate of its population by acuity level for 2016–17. As part of the Governor’s May Revision for 2017–18, the department would submit an updated estimate of its 2016–17 population using actual data available at that time for 2016–17. Based on that updated information, the Legislature could make an adjustment to DSH’s 2016–17 budget. If the population is smaller and/or less acute than initially budgeted for that year, the Legislature would be in a position to revert the corresponding savings to the General Fund. Conversely, if the population is higher than projected and/or more acute, the Legislature could provide additional funding to the department. Additionally, the actual spending and staffing information could also serve as the new baseline. For example if the 2016–17 population was smaller or less acute, the Legislature could base the 2017–18 budget on that smaller population.
Newly Licensed Capacity. We note that newly licensed capacity, such as treatment units the department newly licenses and staffs to accommodate additional patients, require additional resources that would not be accounted for if the budget was adjusted strictly based on the actual population. For example, staff may need to be hired in advance of a new unit being licensed by CDPH, which could result in additional costs and staffing. Therefore, we recommend the Legislature require the department to separately submit requests for any additional funding necessary for new units. Such requests would be in addition to the population–adjusted funding described above.
We believe that our recommended approach for adjusting DSH’s budget has several major benefits. First, it would ensure the department receives an appropriate amount of funding to account for changes in its patient population and the services it provides. Second, DSH would be incentivized to accurately project the patient population and patient acuity levels. Third, the department would have a fiscal incentive to fill all available beds. Fourth, our recommended approach would make DSH’s budget requests more transparent and allow the Legislature to evaluate whether budget adjustments requested by the department to account for population changes are appropriate. While our proposal would likely require additional work for the department in the short run to develop the updated component costs, it would create a more simplified process for the department to develop budget proposals, and for the Legislature to review them in the long run.
We acknowledge that our various recommendations may require time for the department to implement. As such, we recommend that in the interim, the Legislature require DSH to provide additional information to justify any budget requests and address some of the concerns we identified in this report. Specifically, we recommend that the department’s population–driven budget requests be accompanied by additional information to justify those proposals, such as the size and acuity of the patient population and the staffing ratios used for patients of each acuity level. To the extent that any of the proposed staffing exceeds the department’s staffing ratios, DSH should provide justification. This additional information would assist the Legislature in determining the appropriateness of population–driven budget proposals, as well as in making any necessary adjustments to those requests.
Based on our review of the DSH budget process, we find that several improvements can be made to increase the transparency of the process, account for increases in the department’s responsibilities, and increase the operating efficiency of the department and its facilities. We make several recommendations to achieve those goals. Specifically, we recommend budgeting the department for its actual patient population, contracting for an independent review of the department’s staffing, and developing a new, ratio–driven staffing model. We also recommend the Legislature require the department to provide additional justification in the short run to ensure the Legislature has all necessary information to evaluate the department’s budget requests and adjustments.