November 6, 2002
The $2 Billion Question:
Providing Health Insurance for State Employees and Retirees
In recent years, the cost to provide health insurance coverage to state employees and
retirees has increased considerably. The state will pay $1.3 billion for these health
insurance premiums in 2002 and $1.7 billion in
2003. We review actions the Public Employees' Retirement System is taking to control these rising costs and highlight legislative options
to further limit the state and enrollee costs for
the health insurance program. We also recommend steps to further ongoing legislative
oversight of the program.
Introduction
Like many employers, the state provides health insurance coverage for its employees.
In addition, the state provides health insurance
for retirees from state service. The state pays
most of the monthly premiums for this coverage.
In recent years, health care costs have escalated nationwide. A number of factors
have contributed to these increases. Some of these factors are out of the control and influence
of the state as a buyer of health insurance coverage, while other factors are subject to
state control. This report looks at what the
Public Employees' Retirement System (PERS), which administers the state program, is currently
doing to control the state's health insurance costs
for its employees and retirees. It also examines
what the Legislature can do to control these costs.
Throughout this report, we focus on the health program as it impacts the state.
However, these issues and any program changes also would impact local governments that
contract with PERS for health services.
Current Health insurance Program
Administration of the Program
After the federal government, PERS is the second largest public purchaser of
employee health benefits in the nation and the largest
in California. The PERS administers the health insurance program for employees and
retirees of the state, as well as local governments
that contract with PERS to provide this service. Under current law, PERS determines the
health plan design, including:
- The types and level of services covered.
- The level of user fees, or "copays."
- The types of insurance offered—for example,
health maintenance organization (HMO) plans and
preferred provider organization (PPO) plans.
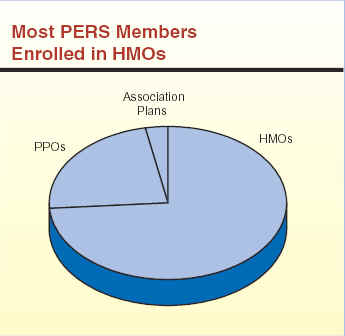
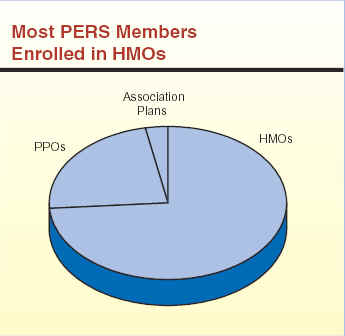
Currently, PERS offers enrollees a choice between seven HMOs and two PPOs. (As
we indicate later, the number of HMOs available to PERS enrollees in 2003 will decline to three.)
In addition, PERS offers three PPO options for specific groups of employees (primarily
highway patrol and correctional officers). Enrollees
who are 65 years of age or older must enroll in
the Medicare-coordinated plans offered by each HMO and PPO. Younger enrollees are
enrolled in the "basic" (non-Medicare) plans. The
health services covered by the participating HMOs
and PPOs are virtually identical. There are more
than 1.2 million individuals covered under the
PERS health insurance program, 60 percent of
whom are state members, with the remainder being local government members.
HMO Versus PPO Plans. There are
important similarities and differences between
HMOs and PPOs. They are similar in that both types
of organizations contract with specific sets of
doctors, hospitals, and other health care providers
to provide services to enrolled members. Also,
both HMOs and PPOs attempt to manage the delivery of health care services to members, although
the extent of this control is less under PPOs.
And herein lies a significant difference between these plans. The HMOs require
the provision of care through a primary care provider who determines whether referrals
to specialists are warranted. By contrast, PPOs permit enrollees to obtain services from
specialists without referral.
Other differences exist between HMOs and PPOs. In general, an HMO enrollee
who receives services outside of an HMO network has to pay the entire costs of those services.
In contrast, the PPO enrollee who obtains services outside of the provider network would not
pay the entire cost of the services, although
he/she would pay a greater portion than if the
service had been delivered by a contracted
provider. Finally, HMOs tend to prepay providers a
per-capita rate for each enrollee (known as capitation), while PPOs generally pay providers on
a discounted fee-for-service basis. Because of these differences, HMO coverage tends to
be less expensive than PPO plans.
The PERS contracts with HMOs (such as Kaiser Permanente and Blue Shield) to
offer HMO plans to employees and retirees at premiums negotiated by PERS and the
individual companies. Thus, these HMOs bear the
financial and legal risk of administering these
health plans if, for example, revenues do not
cover expenses. On the other hand, PERS bears the financial and legal risk of operating the two
PPO plans it offers. This type of arrangement is known as self-insurance and is not
uncommon among large employers.
Premiums Set in Spring for the Next Calendar Year.
The PERS staff negotiates premiums with the HMOs at the beginning
of each calendar year for the following calendar year. These negotiated premiums are
then reviewed and approved by the PERS board during the spring. For example, the
premiums that will be in effect for 2003 were
negotiated and approved during the first part of 2002.
All contracting HMOs must provide the same set of covered services, as designated
by PERS. The negotiated premium for each HMO is the same throughout the health plan's
service area and does not vary from one region of
the state to another.
As indicated above, PERS does not contract with health plans for the PPOs. Instead, PERS
is responsible for administering the program (with the aid of contracted third-party
administrators) and setting premiums at sufficient levels
to cover medical costs. As with the HMOs, the PERS board also sets PPO premiums in
the spring for the next calendar year.
PERS Health Plans, 2002
Health Maintenance Organizations (HMOs)
Blue Shield Access+HMO
Health Neta
Health Plan of the Redwoodsa
Kaiser Permanente
PacifiCarea
Universal Carea
Western Health Advantage
Preferred Provider Organizations (PPOs)
PERSCare
PERS Choice
Association Plans
California Association of
Highway
Patrolmen Health Benefits Trust
California Correctional Peace Officers
Association
Peace Officers Research Association of
California
aNo longer available for 2003. |
 |
State Costs to Provide Health Insurance
Existing law declares that the state's purpose
in providing health insurance to its employees and retirees is to
promote increased efficiency in state government
by (1) attracting and retaining employees
through providing health plans similar to those available
in the private sector and (2) protecting the state's
labor investment by maintaining employees' good health.
In 2002, the total cost (state and employee contributions) of health insurance premiums
for state employees and retirees will be about $1.6 billion. This includes about $1.1 billion
to provide coverage for active employees and their dependents and more than
$500 million for retirees and their dependents. Of the
total amount, the state will pay more than
$1.3 billion while employees and retirees will pay
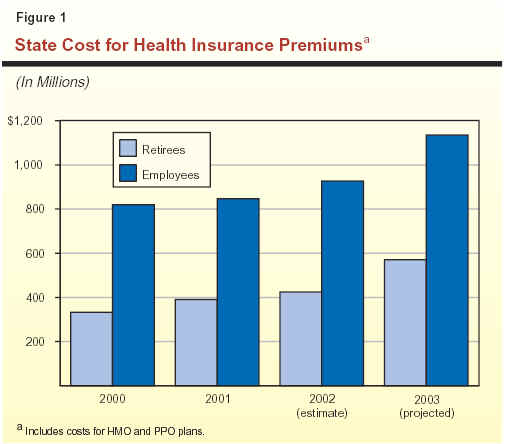
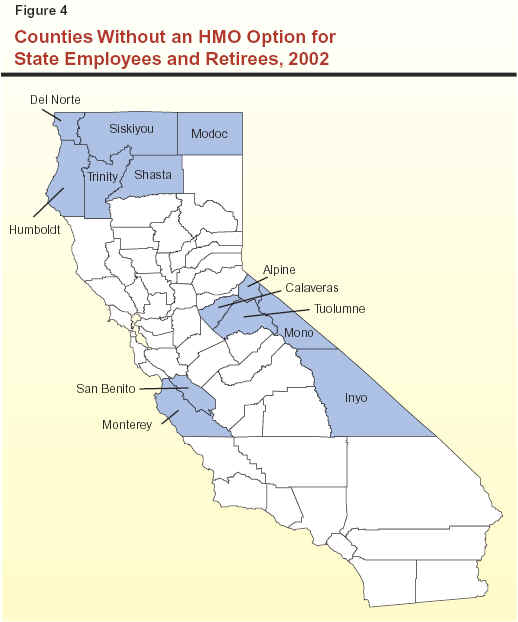
the remainder. Figure 1 shows the growth in
the state's share of costs since 2000.
We estimate that the total 2003 cost for health insurance will exceed $2 billion, with
the state paying $1.7 billion of this amount.
State Contribution for Employees Subject to Collective Bargaining.
Current law requires the state contribution for employees'
health insurance premiums to be determined through collective bargaining. The Department of
Personnel Administration (DPA) establishes the
state contribution for those
employees—including managers and supervisors—who are not
subject to collective bargaining. Under new
memoranda of understanding (MOUs) approved by the Legislature for all 21 bargaining units,
the monthly state contribution for 2002 is $190
for one-party, $378 for two-party, and $494 for family enrollment. This amounts to the
state paying 85 percent of health insurance
premiums for employees and their dependents.
Employees pay the remaining 15 percent.
Statutory Formula Determines State Contribution for Retirees.
On the other hand, current law requires the state to pay
100 percent of a weighted average premium for
retirees and 90 percent of the additional
premiums for their dependents, depending on years
of state service. This is known as the
"100/90 formula." The weighted average premiums
are calculated based on the premiums of the four health plans with the highest enrollment.
This calculation results in monthly state
contributions of $216 for one-party, $411 for two-party,
and $525 for family enrollment in 2002. (If the premium for the health plan selected by
a retiree is lower than these maximums, the state pays the lesser amount.) This amounts to
the state paying 81 percent of premiums for
retirees and their dependents.
State Cost for Employees' Coverage
"Buried" in Departments'
Budgets. While the state annually pays a substantial amount for its
share of health insurance premium costs for state employees, the total cost to the state cannot
be easily identified in the budget. This is
because funding for these costs is spread throughout
the budget. Specifically, the bulk of the state's
cost for employee coverage is included in the base budgets of individual departments, as part
of personal services costs. However, the
additional costs that the state has to pay as health
insurance premiums grow from one year to the next are separately appropriated in a lump sum in
the annual budget act (under Item 9800, Augmentation for Employee Compensation). This
amount supplements the baseline allocations
embedded in individual departmental budgets.
Pursuant to annual budget language, the Department of Finance allocates the
appropriated amount for the higher premiums to
individual departments' budgets. For 2002-03, the budget includes $163 million for the
state's portion of premium increases. When
allocated to individual departments, these
additional health insurance costs also become buried
in departments' baseline budgets in the subsequent year. We estimate that state costs
for current employees (excluding the portion of premiums paid by employees themselves)
are approaching $1 billion in 2002, as shown
in Figure 1.
State Cost for Retirees' Coverage Appropriated in Budget Line
Item. In contrast, the annual budget act includes a line-item
appropriation (under Item 9650, Health and Dental Benefits for Annuitants) for state retirees'
health insurance costs. (Although PERS administers
the program on a calendar-year basis, the state appropriates funding for its share of costs on
a fiscal-year basis.) This provides the
Legislature the opportunity to review these
premium expenditures during budget hearings. The budget includes $577 million for these
state costs in 2002-03.
Additional Program for Higher-Cost Rural
Areas. The total cost to the state to
provide health insurance for state employees and retirees is, in fact, somewhat more than
the $1.3 billion for premiums cited above for
2002. This is because in recent years, HMOs have dropped rural areas from their service
territories for a number of reasons, including the
higher cost of care in those regions compared to urban areas. In particular, factors driving up
rural costs have included greater use of costly
regimens in treating medical conditions and fewer available doctors and hospitals. (Please see
our report HMOs and Rural California for a
more detailed discussion of this issue.) As a
result, state employees and retirees who live in
these rural areas must enroll in one of the
higher-cost PPO plans, which are available
statewide. Consequently, state employee and
retiree enrollment in PPOs has increased.
In order to provide insurance at a similar level of cost to all enrollees (including those
in rural areas), the state established the Rural Health Care Equity program, administered
by DPA. This program subsidizes health care costs for employees and retirees in rural
areas. Generally, the program reimburses (1) out-of-pocket health care costs that would normally be covered by an HMO, such
as deductibles and co-insurance payments (typically a percentage of the cost of service), and
(2) the difference in premiums between the lower cost of the two PPO plans available to
those eligible and the average HMO premium. The budget act includes $32 million for this
program in 2002-03 (under Item 8380, DPA).
The growth in PPO enrollment also drives up the state's health insurance costs in
another way—indirectly, via the weighted average
premium formula used to calculate the state's contribution for retirees' premiums.
Because HMOs have withdrawn from rural areas, one
of the state's PPO plans now is among the top four in enrollment. As a result, this
higher-cost PPO plan now drives up the state
contribution for retirees' premiums at a faster rate
than previous increases.
State Costs Increasing; Will Continue to Escalate
Like other employers, the state has experienced escalating cost trends for health
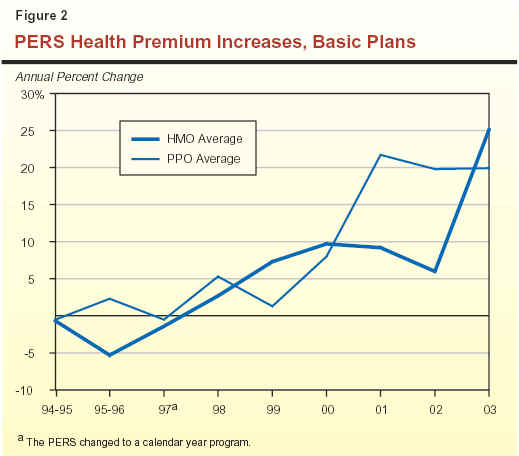
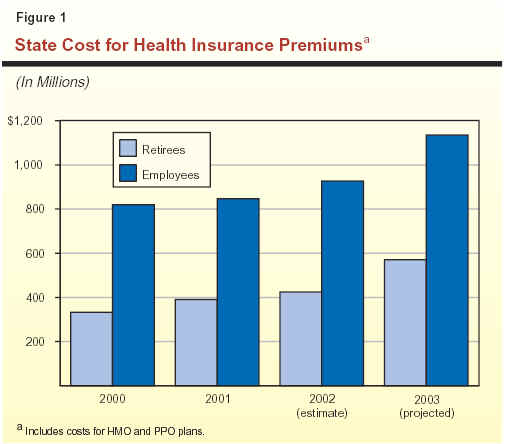
insurance. As a result, premiums have grown considerably in recent years. Figure 2 (see next
page) shows the average premium increases adopted by PERS from the mid-1990s through 2003
for the basic (that is, non-Medicare) HMO and PPO plans.
As Figure 2 shows, HMO premiums have increased by more than 5 percent annually
since 1999. In 2000, the increase approached
10 percent. The increase in HMO premiums dampened for 2002 as a result of plan
changes adopted by PERS to increase enrollees'
out-of-pocket usage fees ("copays") for office
visits and prescription drugs. Without these plan changes, the average HMO premium
increase would have been 13 percent instead of
6 percent. The high 25.1 percent jump for
2003 reflects the current cost pressures on the
health care system, as described below.
Figure 2 shows that from 2000 through 2002, average premiums have increased
even more dramatically for the two PPOs administered by PERS. This reflects mainly
PERS'
efforts to restore the plans' financial solvency,
which has been strained by growing costs and high enrollment growth. The PERS began
these efforts to "catch up" plan reserves in
December 2000. At that time, because of the trend
toward increased levels of treatment and growing enrollment due to
HMO withdrawals from rural areas, the PPOs faced $9 million more in
costs than they had in reserve. In 2002, PPO
premiums increased by an average 19.8 percent, and
PERS adopted a 19.9 percent increase for these
plans for 2003.
Cost Increases Expected to Continue.
Various factors affect the cost of health care.
In recent years, the following factors have
contributed to upward pressure on state health care insurance premiums:
- Increasing cost and use of prescription drugs.
- Higher payments to doctors and hospitals for patient care.
- Greater levels of treatment provided to and used
by patients (including new high-cost technologies).
- An aging population.
These factors are expected to continue driving up the cost of health care and
therefore health insurance premiums.
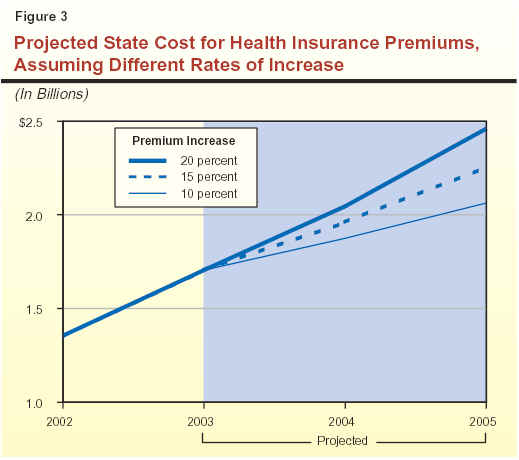
Based on these recent trends, last fall PERS estimated annual premium increases of
15 percent for the HMO and PPO plans from
2003 through 2005, absent changes in program structure. However, recently concluded
premium negotiations for 2003 resulted in much larger-than-anticipated 25.1 percent
and 19.9 percent increases for HMOs and PPOs, respectively, as noted above. Figure 3 shows
the cost to the state if premiums increase at PERS' estimated 15 percent rate for 2004 and
2005, assuming the state continues to pay its
current share of health insurance premiums. The
figure also shows the cost to the state if
premiums were to increase at lower (10 percent)
or higher (20 percent) rates. As shown in the figure, the PERS projection of 15 percent
would result in state costs increasing from
$1.3 billion in 2002 to more than $2.2 billion by 2005.
On the other hand, if premiums increase at a
smaller annual rate of 10 percent, the state's cost
would be just over $2 billion in 2005. An
annual increase of 20 percent would result in
state costs of nearly $2.5 billion by 2005.
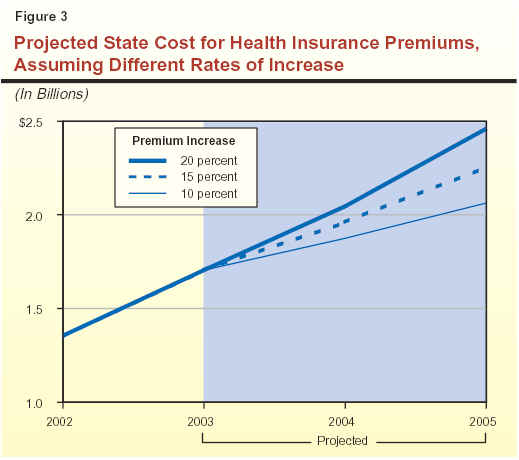
Given the magnitude of these costs, significant dollar savings are possible with even
small reductions in premium growth. Specifically,
a 1 percent reduction in premium costs would save the state around $20 million.
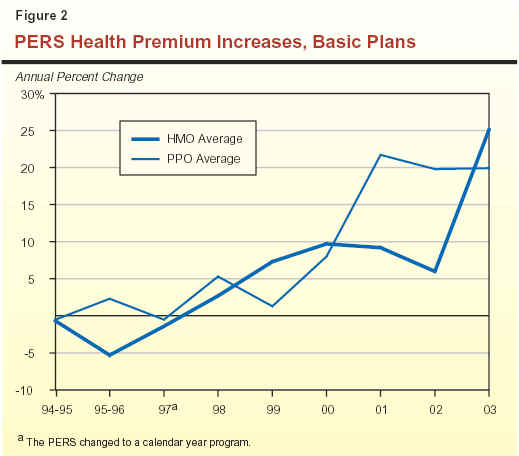
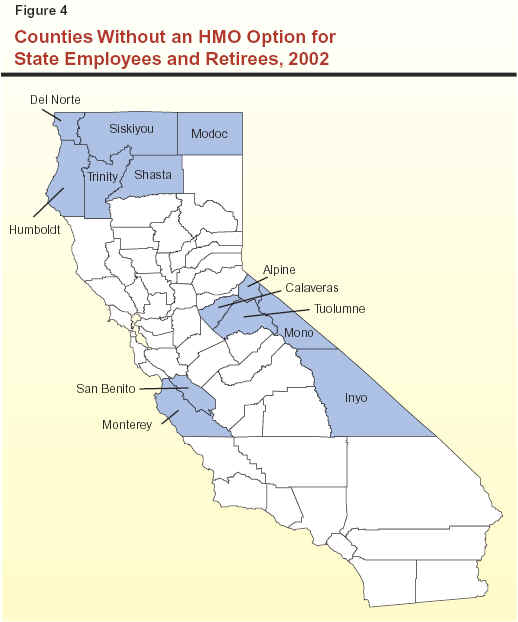
HMOs Dropping Rural Areas Pushes Up Cost.
As discussed earlier, HMOs have dropped certain rural areas entirely from their
service territories because of the higher cost of care
in those regions compared to urban areas. Individuals in these
counties without HMOs must enroll in more costly PPO plans
administered by PERS, which are available statewide.
Figure 4 shows the counties that currently do
not have any HMOs under the PERS program. (There may be
HMOs serving private sector employees in these counties, but not
state employees and retirees.) In 2002, as a result of HMOs leaving rural
areas, state employees and retirees in 13
California counties no longer have an HMO option.
This number will grow to 15 in 2003 with the planned withdrawal of HMOs from Lassen
and Tehama Counties. In addition, parts of nine counties are without an HMO, and this
number will also grow to 15 in 2003.
PERS Attempts to Rein in Growing Costs
Despite its relatively small share of HMO enrollment in California (5 percent to
10 percent for each HMO), PERS has, to date,
been successful at keeping premium increases down. In the 1990s, PERS negotiated very low
premium increases and even reductions in some years. More recently, as discussed
earlier, premium growth has been quite sizable,
largely due to widespread health care cost pressures.
Historically, PERS has successfully negotiated some of the lowest HMO premium increases
in the country. For example, the Kaiser Family Foundation reported that monthly premiums
for private sector employer-sponsored HMO coverage in California jumped 9.9 percent
for 2001, compared to PERS' 9.2 percent
increase. For 2002, federal government employees' health insurance premiums rose
13 percent. Similarly, members of the Pacific Business
Group on Health, which purchases insurance on
behalf of large and small businesses, faced 10 percent
to 20 percent jumps. At the same time, PERS negotiated a 6 percent average premium
increase for its HMOs in 2002.
2002 Premium Negotiations
As part of its efforts to limit cost pressures during HMO contract negotiations for
2002 premiums, PERS rejected the original
proposals submitted by HMOs because of the
magnitude of premium increases requested. Proposed increases for the basic plans ranged from
5.5 percent to 41 percent, averaging
23.3 percent. Instead, PERS required the HMOs to
resubmit lower bids for the existing plan design, as well
as provide bids for two alternative plan designs
that would help limit premium costs. The PERS also announced that it would only contract with
up to seven health plans to be selected based on various performance statistics and price.
Figure 5 shows the weighted average premium
increases for the original and resubmitted bids for
the existing plan design, as well as for the
alternative plan design that PERS subsequently adopted.
|
Figure 5
2002 HMO Premium Bids
Basic Plans
|
|
Proposals
|
Percent
Increase
|
|
Original
|
23.3%
|
|
Resubmitted
|
13.2a
|
|
Adopted (higher copay)
|
6.0a
|
|
|
|
a
Seven adopted HMOs only.
|
In the end, PERS contracted with seven HMOs, eliminating
three from its list of 2001 contracts, and adopted the alternative
design that increased enrollees' copays to further
limit monthly premium increases. Specifically, PERS increased
copays for doctor's office visits from $5 to $10, which
is the most common amount among California businesses,
according to a Kaiser Family Foundation survey. It also implemented
a three-tiered prescription drug copay schedule to encourage enrollees
to use less expensive generic and mail-order drugs. The PERS had
not changed these provisions since the early 1990s.
The PERS estimated that rejecting the initial bids and requiring the health plans to
resubmit new bids lowered total HMO premium costs
for state employees and retirees by
$105 million. Adopting the higher-copay plan further
dropped the premium increase to 6 percent. This
shaved another $82 million off the cost, according
to PERS.
2003 Premium Negotiations
In negotiations for 2003 premiums that would be effective January 1, 2003, PERS
again faced proposals for very high premium increases. Proposed increases for the
existing plan structure averaged 30 percent for the
basic plans. The PERS also requested bids for
alternative plan designs. Alternatives submitted by
the HMOs for consideration included:
- Tiered hospital coverage—with copays ranging from $100
to $1,000 per admission or per day for choosing nonpreferred, more expensive hospitals.
- Changes in prescription drug coverage—with higher
copays (up to 50 percent for brand-name prescriptions) and
higher annual maximum for drug costs paid by the enrollee.
In the end, the PERS board rejected any plan design changes that called for smaller
premium increases and higher out-of-pocket costs
for enrollees. Instead, the board voted to
contract with only the five HMOs with the smallest premium increases, eliminating two HMOs
from its 2002 choices for enrollees.
(Subsequently, two of the five HMOs could not meet
conditional requirements regarding their financial stability and therefore were not included in
the 2003 state program.) This reduced the average premium increase to 25.1 percent. The
PERS estimated that reducing the number of HMOs it contracts with will save $45 million for
state employees in 2003. However, total estimated HMO premiums will still jump by
nearly $300 million to $1.3 billion.
What Else Is PERS Considering?
Beyond its actions relating to the 2002 and 2003 premiums, PERS is pursuing
additional options to rein in growing premium
costs. These options, which are not mutually
exclusive, include the following.
Prescription Drug "Carve-Out."
To address escalating drug costs, PERS is investigating
the feasibility of having a separate carve-out
contract for prescription drug coverage for some or all
of the HMO plans beginning in 2004. Under this arrangement, individual plans would not
provide pharmaceutical coverage. Instead, there
would be a separate contract with one provider to supply prescription drugs for all HMO enrollees.
Currently, one company provides prescription drug coverage for both PPO plans.
By contrast, each HMO provides prescription coverage as part of the plan. Under this
option, bidders for the new contract to provide
prescription coverage to PPO enrollees would have to
be able to serve HMO enrollees as well beginning as early as 2004. Until PERS determines
an estimate of savings from a pharmacy carve-out contract for HMO enrollees, the likelihood
that PERS will implement this option remains unclear.
Data Warehouse Project. The
2002-03 budget includes first-year funding of
$3.5 million for PERS to develop a Health Care
Decision Support System (HCDSS). The project
involves the purchase of off-the-shelf software to
establish a "data warehouse" consisting of
information on the use of medical services and
prescription drugs by those enrolled in the PERS
health program. One-time acquisition costs would
total $6.2 million, with $3.3 million in ongoing
annual costs to support the system beginning in 2004-05.
The PERS indicates that medical and pharmaceutical claims information from HCDSS
would be used to improve patient care and help contain increases in health insurance
premiums by identifying the most prevalent and
costly illnesses, the most effective treatment
regimens, and individual health plans' treatment costs.
The PERS anticipates HCDSS to be functioning in 2004 so that PERS could use data from
the system in negotiations for 2005 health
insurance premiums. Specifically, it is anticipated that
PERS would know actual treatment costs for each HMO with which it contracts. This
information would be used to negotiate premiums
that better reflect actual cost trends. The PERS estimates ongoing premium savings
from HCDSS that would accumulate from year to year—an estimated additional $10 million
in savings each year.
Regional Premiums. The PERS has
also considered adopting some form of
"regional rating" so that premiums reflect the actual
cost of service in various areas of the state.
Currently, each health plan has a uniform statewide
premium schedule for all of its service areas. However, under a regional rating
structure, PERS would divide the state into a number
of regions and allow HMO premiums to vary among regions based on actual treatment
costs. This could induce HMOs to provide services
in higher cost rural areas, and reduce the impact on total premiums resulting from the
withdrawal of HMOs from rural areas.
County-specific information from PERS demonstrates the variability in treatment
costs, which would be reflected, to some degree,
in premium charges under this proposal. For example, per-member monthly HMO
treatment costs range from $109 in the urban south
(San Diego, for example) to $159 in rural areas (Shasta, for example), with a statewide
average of $120. Monthly PPO treatment costs per member range from $171 in the suburban
south (Riverside, for example) to $189 in the
urban north (Contra Costa, for example), with a statewide average of $183.
The HMOs have indicated to PERS that full regional rating, under which premiums
reflect actual costs, may mean that they could stay
in their existing rural areas. This is because
full regional rating would reduce the cost uncertainty associated with HMOs' existing
service territories by allowing the plans to
charge premiums that are in line with their costs
in these more expensive areas. However, HMOs have also indicated that a regional rating
system would not induce them to restore service to areas from which they have already
withdrawn. This is because HMOs have expressed a lack
of interest in reentering high-cost rural areas
under the current PERS program. Consequently, although regional rating could help stem
the tide of HMO withdrawals from high-cost rural areas, it would likely not reverse the
pull-outs that have already occurred.
Fewer Plan Choices, But Statewide Coverage.
The PERS is also considering two major proposals that would further limit the number
of health plan choices of enrollees. These proposals would, however, ensure that the
limited choices are offered statewide, thereby
eliminating the problem of HMOs pulling out of
rural areas. Nonetheless, PERS is only beginning
to develop these proposals and the likelihood of eventual implementation is uncertain at this time.
The first proposal would include three HMO choices with service territories
covering the entire state, instead of HMOs in only
selected parts of the state as is the case
currently. Under the second option, the state would,
like other states and large employers, become self-insured for all enrollees instead of just for
PPO members. The program would offer two or more insurance products (an HMO and a
PPO plan, for example). The PERS estimates significant cost savings for each of these proposals.
Current Law Leaves Legislature Out of the Process
As PERS considers these program design changes, current law leaves the Legislature
out of the process of determining the provisions of the state's health insurance program for its
employees and retirees, as well as how much to pay for it.
PERS Establishes Health Insurance Program.
Existing statute requires the PERS board to
establish the scope and content of health benefits
plans, taking into consideration (1) the "needs
and welfare" of employees and the state and
(2) "prevailing practices" in prepaid medical and
hospital care. No legislative review of the health
plan design is required.
State Cost for Employees Reflects Administration's
Priorities. Under current law, the state contribution for employees'
health insurance—estimated to surpass $1 billion
in 2003—is determined through collective
bargaining. Agreements the administration reaches
with the bargaining units on this item reflect the administration's priorities. Typically,
negotiated MOUs reach the Legislature at the last
minute before the end of session and are often not reviewed in committee hearings. This
occurs despite a statutory requirement that MOU provisions requiring an appropriation must
be approved in the budget act. In practice, the Legislature has little opportunity to
consider state expenditures in this area.
Different Levels of Legislative Oversight Possible
The PERS has over the years successfully negotiated some of the lowest premium
increases among large employers. However, given rising costs in the health care industry,
the Legislature may want to reconsider whether
this broad delegation of authority continues to
meet the state's needs and priorities in the most
cost-effective manner.
There are different approaches the Legislature could use to strengthen its oversight. For
example, the Legislature could take a one-time action to direct PERS to develop
particular coverage choices or have annual budget oversight hearings on health insurance costs
for state employees and retirees. Alternatively,
the Legislature could direct PERS to report on the implications—in terms of cost and
coverage—of the various alternative plan designs that PERS
is currently considering.
Recommend Legislative Oversight On an Ongoing Basis
To provide the Legislature with ongoing information on a multibillion dollar program,
we recommend the following actions.
Annual Report in Budget Hearings.
The Legislature should require PERS to report annually in budget hearings on (1) the
total costs to provide health insurance for state employees and retirees; (2) the trends,
cost factors, and forecasts for the health care
sector; and (3) the steps PERS is taking to
address health care costs and other identified
issues. This would facilitate ongoing legislative
oversight of the program. Based on the information provided by PERS, the Legislature could
also determine on an as-needed basis whether to hold additional in-depth policy and fiscal
hearings. We believe that such oversight hearings are warranted, given that the costs of the
program are increasing dramatically and PERS is moving toward a more consolidated
program structure with fewer plan choices for
enrollees. Both types of hearings would provide
the opportunity for the Legislature to direct
PERS' efforts to reflect legislative priorities and to
make policy changes in the health insurance
program for state employees and retirees.
Consolidated Display in Governor's Budget.
We also recommend that the Governor's budget bring together in one location a
consolidated informational presentation of total
health insurance costs for state employees. This
would improve legislative oversight of total state
expenditures for this purpose. This is similar to how
the state has dealt with expenditures across
multiple departments for the CALFED Bay-Delta program.
Specifically, the informational display should list the number of state employees enrolled
and the cost of health insurance, broken down by (1) HMO and PPO enrollment and (2)
agency. This would make it easier for the Legislature
to identify the growth of program expenditures. Such a consolidated display, together
with budget information currently provided on
health insurance coverage for retirees, would give
the Legislature a more comprehensive picture of the state's health insurance costs for current
and past employees.
Legislative Options to Limit Costs
In addition to increasing oversight, we identify two primary ways that the
Legislature could limit total costs for employee and
retiree health insurance premiums paid both by the state and by enrollees. The first
approach focuses on developing lower-cost HMO options. This approach emphasizes the
development of health plan choices that limit
total premiums—both those paid by the state and
by enrollees. The second option changes the way state contributions are determined. In particular,
it focuses on the collective bargaining process
and the statutory formula for retirees.
Develop Lower-Cost HMO Options
In structuring the state's health insurance plans, PERS, unlike some states such as
Missouri and Oregon, has required that contracting HMOs offer a
standardized package of services that are covered with specified copays.
Thus, the HMOs compete with one another only on price and quality of service provided, not on
the types of services offered.
As a result, unlike other forms of insurance such as auto or homeowners' coverage,
enrollees do not have any option within the HMO choices to decide how much insurance
they want. For example, enrollees cannot choose a plan that reduces their monthly premiums
by having fewer covered services, a $100 or $250 per-admission copay for hospitalization
or surgery, or a higher copay for doctor visits.
To offer more consumer choice and potential premium savings for enrollees and the
state, the Legislature could examine the feasibility
of offering an alternative, lower-cost health
insurance option to state employees and retirees. Such an option, for example, could require
each contracting HMO to provide one lower-cost and one higher-cost plan to enrollees, instead
of just one standardized plan. (Although PERS required HMOs to submit proposals with
two plan designs for 2002, the differences
included only relatively minor changes in doctor visit
and prescription drug copays.) In fact, the
current two PPO plans are already structured in such
a manner. One plan offers lower monthly premiums than the other in exchange for greater
cost sharing for medical services. Specifically,
the lower-premium PPO generally requires enrollees to pay 20 percent of health care costs up
to a specified amount, whereas the higher-premium plan requires enrollees to pay just
10 percent of health care costs.
The lower-cost options would reduce enrollees' out-of-pocket premium costs to
the extent the plan's premium is above the maximum state contribution. In addition,
these options could reduce state contributions to
the extent that there are more plan options that
cost less than the maximum state contribution. However, developing lower-cost HMO
options would not address the lack of HMO coverage in rural areas.
Change the Way State Contributions Are Determined
There are also a number of ways that the Legislature could change how the state
contributions for health insurance premiums are derived, with the potential for reducing
state costs depending on how the changes are structured.
Adopt Formula for State Employees.
Prior to 1974, state law prescribed a specific
dollar amount (increased periodically) as the
state's share of employee health insurance
premiums. In 1974, the Legislature changed the
state's contribution for health insurance to
80 percent of the average premium for employees
and retirees and 60 percent for their
dependents. This formula was subsequently increased to 85/60 in 1975 and finally to 100/90 in 1978. However, in 1978, the Legislature also
allowed the state contribution for employees'
health insurance premiums to be determined through collective bargaining, which typically
concludes after the budget is completed. Unlike state
costs for retirees which is governed by the 100/90 formula, the state's cost for employees
is unknown when the budget is approved.
While total cost is a significant issue with
this program, the uncertainty of how much the
state will pay is another key issue. To eliminate
some uncertainty regarding the amount the state
has to pay for its employees, the Legislature
could again adopt a formula for calculating the
state contribution for employees. In fact, the
Legislature recently attempted to do this. In 2001,
the Governor vetoed AB 1554 (Hertzberg), which would have applied the 100/90 formula to
state employees. The PERS estimated that this
would have cost an additional $64 million in 2002,
or about 7 percent of current state
expenditures for employee health insurance.
The Legislature could consider a contribution formula for employees other than the
100/90 formula envisioned by AB 1554. A formula resulting in reduced state costs
would not be outside the norm for contributions by California businesses, the state itself in the
past (as noted above), or other states. In 2002,
PERS estimates that the state will pay an amount
equal to 85 percent of total health insurance
premiums for employees and their dependents.
According to a 2002 Kaiser Family Foundation
survey, businesses in the state pay the equivalent
of 90 percent of one-party premiums and
79 percent for family enrollment. In addition, a
2001 survey of state government health benefits reported that a majority of states cover less
than 75 percent of dependent premiums. Thus, California pays a similar portion of
employee and dependent premiums as businesses in
the state, but a higher portion of dependents' premiums than other states.
We also did a nationwide survey of states, of which 14 responded. Our survey shows that
of the responding states, most pay a greater portion of employee premiums but a
smaller portion of dependent premiums than
California does (see Figure 6). In addition, only five
negotiate state contributions through the
collective bargaining process. Specifically, a number
of states including Iowa, Maine, Oregon, and Texas pay 100 percent of employee
premiums and anywhere from zero to 80 percent
of dependent premiums. Others like Nebraska, Nevada, and Vermont pay the same
portion, ranging from 75 percent to 80 percent,
for employees and their dependents alike. New York pays 90 percent of employee
premiums and 75 percent of dependent premiums.
Drawing from these findings, if the state adopted an 85/75 formula for employees
and their dependents, we estimate that state
savings in 2003 would be about $16 million.
Alternatively, with a 100/50 formula, the state
would save approximately $70 million.
Adopting a statutory formula would not impact overall premium increases. Rather,
it would determine what portion of premiums would be paid by the state. In addition,
depending at what level a formula is fixed and what
the administration would have otherwise negotiated in collective bargaining, it would also not
necessarily reduce state premium costs. It would, however, eliminate some uncertainty
regarding how much the state will pay from year to year.
Change 100/90 Formula for Retirees.
Our survey shows that while 8 of the 14 states
listed in Figure 6 pay some contribution for
retirees' premiums, only four of them contribute
toward dependent premiums. In comparison,
California uses the 100/90 formula to calculate the
state portion of premiums for retirees and their dependents.
|
Figure 6
LAO Survey of State
Contributions for Health Insurance Premiums
|
|
|
Employees
|
|
Retirees
|
|
|
State
Pays Less Than California For . . .
|
|
|
Coverage
Provided For . . .
|
|
Respondent Statesa
|
Employee
|
Dependents
|
Collectively
Bargained
|
|
Retiree
|
Dependents
|
|
Iowa
|
|
ü
|
ü
|
|
|
|
|
Maine
|
|
ü
|
b
|
|
ü
|
|
|
Mississippi
|
|
ü
|
|
|
|
|
|
Missouri
|
ü
|
ü
|
|
|
ü
|
|
|
Nebraska
|
ü
|
ü
|
|
|
|
|
|
Nevada
|
ü
|
ü
|
|
|
ü
|
ü
|
|
New York
|
|
ü
|
ü
|
|
ü
|
ü
|
|
North Dakota
|
|
ü
|
|
|
ü
|
|
|
Oregon
|
|
ü
|
ü
|
|
|
|
|
Texas
|
|
ü
|
|
|
ü
|
ü
|
|
Utah
|
|
|
|
|
|
|
|
Vermont
|
ü
|
ü
|
ü
|
|
ü
|
ü
|
|
Washington
|
|
|
|
|
c
|
|
|
Wyoming
|
|
ü
|
|
|
|
|
|
a
Respondents to LAO nationwide survey.
|
|
|
b
Maine's contribution for dependents is determined through
collective bargaining.
|
|
c
Washington pays a specified dollar amount for retirees
enrolled in Medicare.
|
As discussed previously, the state provides health insurance for its employees—both
active and retired—in order to attract and retain
them and to protect this labor investment. This is
to help achieve the goal of having a more efficiently run government. While the prospect
of having state-paid health insurance in
retirement may influence some to work for the state,
we find little analytical basis for the state to
contribute more for retirees' health insurance
premiums than for current employees' premiums. However, this is precisely the case, as shown
in Figure 7.
|
Figure 7
2003 State Contributions
for
Health Insurance Premiums
`
|
|
Enrollment
|
Employeesa
|
Retireesb
|
|
One-party
|
$226
|
$288
|
|
Two-party
|
449
|
537
|
|
Family
|
587
|
665
|
|
|
|
a
Determined by collective bargaining.
|
|
b
Determined by the 100/90 formula.
|
State expenditures for retirees' health insurance have jumped 33 percent since
2000 to an estimated $424 million in 2002 because
of both enrollment and premium growth. To control this expenditure growth in the future and
to create a more balanced relationship between state contributions for employee and
retiree premiums, the Legislature could change the
100/90 formula as discussed in more detail below.
However, it appears that the formula could only be changed prospectively—that is, for
state employees beginning service after the
formula changes. This is because court decisions
have often considered employer contributions for retirees' health benefits to be part of the
employment contract as guaranteed compensation. As a result, changing this contribution for
current employees and retirees is likely to be
determined by a court to be a contract violation.
The Legislature has prospectively changed this contribution in law twice before. From
1978 through 1984, the 100/90 formula applied to
all current and future retirees. Then the
Legislature changed state law for employees first hired
on or after January 1, 1985. These individuals
would not be eligible for the full amount of the
100/90 formula contribution in retirement until
they worked for the state for ten years (instead
of five years as under prior law). Another law change effective January 1, 1989, made
new employees starting after that date eligible for
just half of the 100/90 formula contribution in retirement after ten years of state service.
These individuals would then be eligible for an
additional 5 percent of the formula amount
with each additional year of state service, up to
the full amount after working for the state for 20 years.
The Legislature could similarly adopt another contribution schedule for retirees to
apply to new state employees hired after some
future date. Alternatively, the Legislature could set
the state's monthly contribution for retirees'
health insurance premiums at the same dollar
amount as that negotiated for employees through collective bargaining. Any savings would
be prospective though, once those new employees retire. Thus, there would be no
near-term savings from changing the contribution
for retirees now.
Strengthen Incentive to Choose Lower-Cost Plans.
The Legislature could also consider significantly strengthening the incentive for
both employees and retirees to select lower-cost
plans. One way to achieve this is by setting the
state's contribution at some portion of (or equal to)
the monthly premium of the lowest-cost plan
available in each county. (The state contribution
may vary depending on what plans serve each county.) While PERS requires health plans
to meet certain standards to be approved for the state program, the premiums vary from one
plan to another. The Legislature could send a
strong, clear signal encouraging employees and
retirees to choose lower-cost health plans by tying
the state contribution to the lowest-cost plan
available. If individuals believe that other
options provide better care or otherwise better
meet their needs, then they could pay the
difference in premium for a more expensive health plan.
We recognize that this option could cause the state contribution for health insurance
to vary by county to the extent that the
lowest-cost health plan is not offered statewide. For
example, because it lacks HMO service, the state contribution for employees and retirees
in Trinity County would be tied to the premium of the lower-cost PPO plan available there. On
the other hand, the state contribution in Ventura County would be tied to the lowest-cost
HMO plan available there, which has a smaller premium than the PPO plans. Thus, the
state contribution in Trinity County would exceed that in Ventura County if such an option
were currently in effect.
Such variation in compensation is not without precedent. For example, the
state currently offers pay differentials for
hard-to-fill positions based on criteria such as
location. Varying the state health insurance
contribution based on available health insurance
choices would similarly reflect local economic and employment conditions.
If implemented, this option should be coordinated with the existing Rural Health
Care Equity program. This would avoid compensating eligible employees for the HMO-PPO
premium differential already addressed by the higher
state contribution for rural areas that would be adopted under this option.
Other Options
There are other options the Legislature may wish to consider or have PERS investigate.
For example, the state could consider
consolidating prescription drug purchasing for all state
departments. Currently, PERS contracts for
prescription coverage for state employees and
retirees, while the Department of General Services contracts on behalf of other departments
such as Corrections, Mental Health, and Developmental Services for their prescription
drug needs. In addition, and at a more macro
level, the Legislature may wish to study the
feasibility of consolidating the state's separate
purchases of health insurance coverage for programs
such as PERS, Medi-Cal, and Healthy Families.
These options may help maximize the state's
negotiating leverage as a large purchaser of
health coverage, thereby enabling the state to
achieve better prices and lower costs.
Conclusion
The PERS is taking a number of steps to help control the sharply rising cost of the state
health insurance program for employees and
retirees. We recommend ongoing legislative oversight
of this program. Specifically, we recommend:
- An annual report from PERS in budget hearings on (1) the
total costs to provide health insurance for state
employees and retirees, (2) health care cost trends and forecasts
generally, and (3) PERS actions to address growing program
costs and other identified issues.
- A consolidated informational display of total health insurance costs for
state employees in the annual Governor's budget.
We have also highlighted two major options for the Legislature to consider to further
limit state and enrollee costs for the program:
- Develop lower-cost HMO options.
- Change the way state contributions are determined.
| Acknowledgments
This report was prepared by ,Todd
Clark, under the supervision of C.
Dana
Curry. The Legislative Analyst's Office (LAO) is a nonpartisan office
which provides fiscal and policy information and advice to the
Legislature. |
LAO Publications
To request publications call (916) 445-4656.
This report and others, as well as an E-mail
subscription service, are available on the LAO's Internet site at
www.lao.ca.gov. The LAO is located at 925 L Street, Suite 1000,
Sacramento, CA 95814. |
Return to LAO Home Page