Executive Summary
Chapter 7, Statutes of 2009 (ABX4 7, Evans), directs the Department of Health Care Services (DHCS) and the Department of Social Services (DSS) to implement a statewide eligibility and enrollment determination process for the California Work Opportunity and Responsibility to Kids (CalWORKs), Food Stamp, and Medi–Cal programs. The new statewide process is intended to achieve two primary outcomes: (1) providing better service to people applying for these programs and (2) lowering administrative costs through better use of technology.
Main LAO Findings
Opportunities Exist to Improve Current Processes. Our analysis indicates that there are a number of potential improvements to the current eligibility and enrollment determination processes that the Legislature should consider. These include implementing online application processes, simplifying documentation of eligibility, simplifying eligibility rules, use of document imaging technology, and better integration of technology systems.
Evaluating the Potential for Savings. The General Fund costs for program administration for the programs discussed above have grown to exceed $1.5 billion annually. The administration’s estimate that the state could save $500 million from the General Fund annually is probably overstated and does not take into account program cost increases associated with simplification of eligibility. However, less but still meaningful levels of savings may be achieved through changes in enrollment and eligibility processes.
Thinking Through Consortia Strategies. The Legislature is also facing major, costly decisions about the future of the county–operated automation systems (known as consortia) that support eligibility and enrollment functions for these key health and social services programs. These include decisions about whether to launch a project to replace the Los Angeles County consortium and about how many consortia the state will support in the future.
Creating Buy–In. Counties are a critical partner in the state’s administration of the CalWORKs, Food Stamp, and Medi–Cal programs. Absent the creation of appropriate incentives, counties may lack sufficient motivation to undertake the sometimes–difficult changes to improve the efficiencies of the eligibility and enrollment processes for these programs.
A Roadmap for the Legislature
As the administration continues its stakeholder process to develop a plan to implement Chapter 7, we recommend a general approach the Legislature may wish to consider to navigate these difficult decisions.
Prioritize Changes That Improve County Efficiency. We recommend that the Legislature direct the state departments, in conjunction with the Health and Human Services Agency (HHSA), to work collaboratively with counties to prioritize some of the improvements that would increase the efficiency of counties’ administration of the eligibility processes for these programs.
Assess Requirements of Federal Health Reform. The Legislature should direct HHSA and DHCS to assess the requirements of federal health care reform on the state‘s eligibility and enrollment determination processes for its health programs.
Provide a Fiscal Incentive for County Cooperation. The Legislature should direct the state departments and HHSA to incorporate a strategy for sharing cost savings with counties to help ensure county buy–in for the successful implementation of improvements in eligibility and enrollment processes.
Be Aware Certain Improvements Likely to Increase Caseload. An increase in enrollment in Medi–Cal and CalWORKs will result in increased state benefit costs, which, given the state’s fiscal condition, may not be in the state’s best interest at this time. Accordingly, we recommend that the Legislature require the departments to conduct a cost–benefit analysis of the impact of implementing various front–end strategies.
Build in Flexibility for Future Improvements. We recommend that any new eligibility and enrollment systems be developed with the flexibility to incorporate changes in the future, such as making significant reforms to the eligibility process and allowing an improved interface with other databases to verify eligibility documents.
Consider the Future of the Consortia Systems. We recommend that the Legislature continue to take steps to reduce the number of consortia systems over time.
Introduction
Chapter 7 directs DHCS and DSS to explore and potentially implement a statewide eligibility and enrollment determination process for CalWORKs, Food Stamp, and Medi–Cal programs. The new statewide process is intended to achieve two primary outcomes: (1) providing better service to people applying for these programs and (2) lowering administrative costs through better use of technology.
Chapter 7 requires the departments to develop a plan for an improved eligibility system. The plan’s required components are similar to state requirements for new information technology (IT) projects and include a project description and a cost–benefit analysis of procuring a system compared to building upon existing systems. The plan must be submitted to the Legislature at least 45 days prior to a request for an appropriation to implement such a new process.
The administration is currently taking some first steps to implement Chapter 7. Among other actions, it is conducting meetings with key stakeholder groups, as the legislation requires, to determine the best approach for reforming the administration of CalWORKs, Food Stamp, and Medi–Cal eligibility and enrollment processes.
Programs Targeted for New Statewide Process Have Similar Populations and Processes
The CalWORKs, Food Stamp, and Medi–Cal programs serve similar populations, require applicants to go through somewhat analogous steps to apply for benefits, and rely on the same automation systems to manage data and support the eligibility determination and enrollment processes. In spite of these commonalities, the eligibility determination and enrollment processes for the individual programs are complex and vary significantly for each program mainly due to mandates in state and federal law. The populations served by each of the programs, as well as the general steps in their eligibility and enrollment determination processes are described below.
Target Programs Serve Similar Populations
Because the CalWORKs, Food Stamp, and Medi–Cal programs serve similar low–income populations, some individuals enroll in all three. Figure 1 provides a brief description of each program and highlights some of the key similarities and differences in eligibility requirements.
Figure 1
Target Programs Serve Similar Populations and Have Similar Eligibility Requirements
|
|
CalWORKs
|
Food Stamps
|
Medi–Cal
|
|
Program description
|
Provides cash grants and welfare–to–work services to low–income families. Grants vary by family size, location, and income.
|
Provides benefits to low–income households and individuals for food purchases. Monthly benefits based on household size and income.
|
Provides health care services to low–income persons, primarily families with children, and seniors and persons with disabilities.
|
|
2009–10 caseload
|
546,000 households/1.3 million individuals
|
1.3 million households/3.1 million individuals
|
7.3 million individuals
|
|
Income limits
|
Yes
|
Yes
|
Yes
|
|
Asset limits
|
Yes
|
Yes
|
Yes
|
|
Work requirements/training/education
|
Yes
|
Yes, for certain cases.
|
No
|
|
Face–to–face interview required?
|
Yes
|
Yes, but individual counties can waive the face–to–face interview.
|
No
|
|
Fingerprinting
|
Yes
|
Yes
|
No
|
|
Status reports
|
Quarterly
|
Quarterly
|
Children: annual; adults: midyear
|
Steps in the Eligibility and Enrollment Processes Are Similar
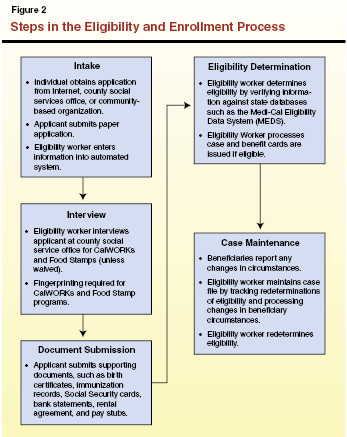
The general steps involved in the eligibility and enrollment determination process for the CalWORKs, Food Stamp, and Medi–Cal programs are illustrated in Figure 2. The amount of time it takes an applicant to receive benefits after an application has been submitted depends on individual program requirements, timely submission of documents by the applicant, and timely processing of applications by the eligibility worker. Families receiving CalWORKs benefits are automatically eligible for Medi–Cal. Although the three programs generally share similar income eligibility requirements, they differ in other eligibility requirements. For example, the CalWORKs and Food Stamp programs require fingerprinting, but Medi–Cal does not.
County staff performs most of the eligibility determination and enrollment activities and the state and federal government provide funding for their efforts. We estimate that, in 2009–10, counties will receive $3.4 billion ($1.4 billion from the General Fund) to administer the eligibility determination and enrollment processes for CalWORKs, Food Stamp, and Medi–Cal programs, as shown later in this report in Figure 4.
Many Automation Systems Support Eligibility and Enrollment
The Consortia and Other Automation Systems
As we present below, the CalWORKs, Food Stamp, and Medi–Cal programs are supported by many different automated systems that enable case management and administration of program benefits, among other functions. These automation systems rely on a mix of federal, state, and county funding. A summary of these systems and their annual ongoing maintenance costs is shown in Figure 3.
Figure 3
The Statewide Automated Welfare System
(General Fund,a in Millions)
|
|
Maintenance and Operation Costs
|
|
2009–10
|
2010–11
|
|
Interim Statewide Automated Welfare System (ISAWS) operates in 35 smaller counties. These counties are currently migrating to Consortium IV (C–IV). The four–year migration costs are estimated to be $250 million (all funds).
|
$12.7
|
$12.9
|
|
Los Angeles Eligibility Automated Determination, Evaluation, and Reporting System (LEADER) serves Los Angeles County (one–third of the state’s caseload) and is currently in a procurement for a replacement system. The LEADER project plans to award a contract to a vendor at the beginning of 2011. The LEADER replacement project is estimated to cost $530 million (all funds).
|
6.4
|
6.4
|
|
CalWORKs Information Network (CalWIN) operates in 18 counties (about one–third of the state’s caseload) and cost almost $600 million (all funds) to develop. Its current contract for maintenance and operation will end in 2013. Project staff are planning a competitive procurement for continued maintenance and operations services beyond the life of the current contract.
|
36.6
|
38.8
|
|
Consortium IV serves four counties and cost over $300 million (all funds) to develop. After all ISAWS counties migrate to C–IV, it will serve 39 counties, about one–third of the state’s caseload. Implemented in 2004, C–IV is the only consortia with a Web portal, allowing customers to submit online Food Stamp applications. The C–IV project is planning to reprocure its maintenance and operations services in late 2011.
|
24.5
|
24.6
|
|
Totalsb
|
$80.2
|
$82.7
|
Statewide Automated Welfare Systems (SAWS). Four county–operated automation systems (called consortia) make up SAWS. The consortia support eligibility and benefit determination, enrollment, case maintenance, and statistical reporting, among other functions at the county level for various health and social service programs. The Legislature originally approved the development of four consortia in the 1995–96 Budget Act after the state had attempted for several years to design and build a single statewide system. At that time, the Legislature determined that it wanted no more than four county consortia and in 2006 further expressed a preference for reducing this number when it decided to migrate certain counties to an existing system rather than procure a new system. As discussed later in this report, the interim statewide automated welfare systems (ISAWS) consortium will migrate into the C–IV consortium in 2010, leaving the state with three consortia.
Each system cost several hundred million dollars to develop. Their annual maintenance and operations cost a total of $152 million when all fund sources are considered (with about $80 million coming from the General Fund). Because the state operates multiple consortia, it needs other systems which reconcile statewide issues. For example, the Welfare Data Tracking Implementation Project (WDTIP), while not a consortium system, is the interface with the existing SAWS that tracks and reports time–on–aid for CalWORKs’ recipients. Annual maintenance costs for WDTIP are about $4 million.
Medi–Cal Eligibility Data System (MEDS). The MEDS is a statewide automated database that houses data about applicants, such as their enrollment in other public assistance programs. Each of the consortia can interface with MEDS, although the process of relaying data back to counties in response to requests about particular applicants can sometimes take one or more days. The annual maintenance and operations cost for MEDS is about $18 million. It will likely need to be modernized and redeveloped in the next few years as it is over 30–years old and relies on old technology that is difficult and time–consuming to modify.
Income and Eligibility Verification System (IEVS). The IEVS is used to verify whether the income information that applicants provide during intake matches the income information contained in other databases, such as the Payment Verification System administered by the state Employment Development Department and the U.S. Social Security Administration. The IEVS enables eligibility workers to verify only an applicant’s historical income, as the information generally lags by six months. The annual system maintenance costs for IEVS was about $400,000 in 2008–09.
Electronic Benefit Transfer (EBT) System. The EBT provides an automated system for the electronic payment of various types of public assistance benefits, including federal food stamps, CalWORKs cash grants, refugee cash assistance, and general assistance. As indicated, EBT supports many different social services programs and must interface with the four county welfare consortia. In late 2009, a new contract for EBT services was procured in anticipation of the expiration of the current contract in August 2010. Total reprocurement costs are estimated to be $47 million. Annual maintenance costs for the system are expected to be $27 million.
Statewide Fingerprint Imaging System (SFIS). The SFIS is used to detect fraud in the CalWORKs and Food Stamp programs (as well as the In–Home Supportive Services program, under recent legislation) by matching the fingerprints of program applicants against a database containing fingerprints of persons who are already receiving aid. A new contract for services to maintain and operate SFIS was procured, and annual maintenance costs are expected to be about $12 million.
Other Systems. Counties also use their own local IT systems (generally spreadsheets and databases) to support the systems described above. These systems tend to be developed in–house by county IT staff (rather than purchased from a vendor) and are county funded. They often provide staff with “workarounds” to the other systems described above that may not be flexible enough to handle county–specific processes. For example, a social services office in Sacramento County developed an Access software program database to track Medi–Cal applications for that county that originated through a centralized application system operated by the state called the “single point of entry.”
Drawbacks of the Current Processes and Automation Systems
The current processes for eligibility and enrollment determinations for the CalWORKs, Food Stamp, and Medi–Cal programs, along with the automation systems that support these processes, have a number of drawbacks. For example, the current eligibility and enrollment process does not fully harness currently available technology (such as the scanning of documents needed to verify program eligibility and allowing applicants to submit such information via the Web) to make the application process more convenient. Additionally, no processes now exist to tap into the information available in existing state and other databases for asset, income, and other information that could minimize the burden on applicants of gathering supporting documentation that the eligibility worker must then verify.
The state’s automation systems to support these programs are costly for the state to develop and maintain, in part because the state has so many separate consortia as well as so many ancillary IT systems that interface with these consortia. Moreover, information cannot be shared among and within consortia. This makes it difficult for applicants who move between counties to continue receiving benefits for which they are eligible without disruption, or for eligibility workers to detect fraudulent applications for individuals seeking the same benefits from multiple counties. Additionally, the operation of so many different IT systems creates a lack of standardization of the eligibility determination process across the state, which could lead to variations in eligibility determinations. Such variation could result in eligible applicants in one county not receiving services, while ineligible applicants in another county may receive benefits. Furthermore, some of the existing systems (such as MEDS) are outdated or contain information that is not current (such as outdated income information in IEVS), contributing to a lengthier application process, lags in the receipt of benefits, and the potential for ineligible applicants to receive benefits.
Some Progress Being Made in the Consortia Systems
Counties in each of the consortia acknowledge the drawbacks described above and are attempting to address some of them. For example, consortia IT staff, along with their respective vendors, are developing ways to allow applicants to apply for program services online and via the phone. Additionally, many counties are procuring document imaging systems. Consortia have been able to fund these technology enhancements using a combination of federal and private grants and existing maintenance and operation dollars.
Opportunities Exist to Further Improve Current Processes
The processes and automated systems described earlier are complicated for program applicants to navigate and administratively burdensome for county eligibility workers. Below, we summarize some of the potential improvements in the current eligibility and enrollment processes that we believe the Legislature should consider. These best practices generally fall into two categories: (1) “front–end” improvements that facilitate access to program benefits and simplification of the application process and (2) “back– end” improvements that would make the eligibility determination process more efficient.
Front–End Improvements
Online Application Processes. As described above, many counties already have or are implementing processes that would enable individuals to apply for certain benefits online from any computer with an Internet connection, as well as via the phone. Data is transmitted directly into the county offices’ automated systems, eliminating the need for eligibility workers to manually enter data from paper applications.
Each of the three consortium systems are separately working to develop technologies to allow for an online application process. For example, an online application program for the Consortium IV (C–IV) counties called C4Yourself allows applicants to apply online (at www.c4yourself.com) for benefits under the CalWORKs, Food Stamp, and Medi–Cal programs. The data from the application form uploads directly into the system and does not require manual data entry by county staff. Eligibility workers review the data for completeness and accuracy. Also, CalWORKs Information Network (CalWIN) and Los Angeles Eligibility Automated Determination, Evaluation, and Reporting System (LEADER) are working on implementing similar processes. In efforts which predate enactment of Chapter 7, the state’s HHSA has been exploring plans for a statewide portal that will allow individuals to apply online for the CalWORKs, Food Stamp, and Medi–Cal programs, as well as several other health and social services programs. This statewide portal would interface with each of the consortia systems.
These front–end improvements could go a long way in streamlining the initial application process for beneficiaries and county workers. In the future, applicants may be able to verify their eligibility for benefits by electronically signing an oath under penalty of perjury, potentially allowing the realization of event greater front–end efficiencies.
Simplifying the Burden of Documentation. Another type of front–end improvement focuses on lessening the burden to applicants of the time–consuming process of gathering the documents that are ordinarily needed (such as birth certificates and bank statements) to verify their eligibility for benefits. This alternative approach relies on accessing information through electronic systems about their income and assets that could affect their program eligibility. For example, information about the finances of applicants could be obtained from credit reporting agencies. The Department of Motor Vehicles maintains information that could be used to determine whether an applicant owned a motor vehicle.
Simplification of Eligibility Rules. The application process could be changed so that applicants would no longer be required to submit some documentation of their income, such as pay stubs. Applicants could instead be allowed to “self–certify” their income, assets, and household characteristics by signing under penalty of perjury. While this approach may raise issues about the accuracy of the information provided, the state would continue to be responsible for verifying the information. This could be done through more automated means, such as accessing the credit records of applicants. Studies have found this approach decreases administrative costs, reduces the burden on applicants, and increases enrollment. Eligibility rules could also be simplified by allowing continuous eligibility for adults—meaning, that an individual would be enrolled in Medi–Cal for up to one year before they would have to again validate whether they were still eligible for the program on the basis of their income. We would note that some of the rules regarding eligibility for the state’s health programs (such as the elimination of the asset test for certain individuals) may change as a result of the recently enacted federal health care reform.
Back–End Improvements
Document Imaging Technology. One type of back–end improvement involves converting paper documents such as birth certificates, pay stubs, and immunization records that must be submitted by applicants into digital images. Because the images are digital, they can be easily stored and shared. For example, when a person determined eligible for CalWORKs also submits an application for Food Stamps, the same documentation could be used again to confirm an applicant’s eligibility for the second program. Document imaging is currently being used throughout the C–IV counties, in all but two CalWIN counties, and to a lesser degree in Los Angeles County. We note that, in addition to making the process of determining eligibility more efficient, document imaging technology could also improve the front–end application process if applicants were allowed to submit electronically documents needed to verify their eligibility.
Better Integration Within and Among Counties. Use of newer technology could allow electronic information to be exchanged within counties and among the consortia systems. Through better system integration, counties could share basic information submitted by the applicant for the eligibility determination process, such as pay stubs and immunization records. This would allow an eligibility worker to obtain an applicant’s historical record from another county and use the information to complete a new application in less time.
Implications of Federal Health Care Reform
On March 23, 2010, President Obama signed into law the Patient Protection and Affordable Care Act (H.R. 3590 with its companion set of amendments in H.R. 4782), which is designed to provide health coverage to 32 million people nationwide. At the time this analysis was prepared, federal agencies were just beginning the process of developing regulations and processes to implement these and other provisions of the new federal health care reform package. However, the impact of these changes in federal law is likely to be significant, as the reform package requires the state to implement a “no wrong door” process. This means that state would have to allow all individuals seeking health coverage through certain programs to be screened for eligibility for all programs and referred to the appropriate program for enrollment, without submitting additional materials or undergoing multiple eligibility determinations. States will be required to establish an enrollment website and use electronic interfaces and data matches with existing databases and other programs to verify eligibility at enrollment and renewal. In addition, asset tests are eliminated for all Medicaid beneficiaries, except those applying for long–term care services.
Evaluating the Potential for Savings
One of the statutory goals of changing eligibility and enrollment systems established in Chapter 7 is to reduce the costs of administering the CalWORKs, Food Stamp, and Medi–Cal programs. The administration has estimated that carrying out the changes contemplated in the measure would result in state General Fund savings of up to $500 million annually ($1 billion all funds). In our analysis below, we discuss the significant costs the state is now incurring for these systems and assess the potential for such savings.
Current Costs of Eligibility and Enrollment Systems Exceed $3.6 Billion
Figure 4 shows the 2009–10 funding levels for the county administration of the CalWORKs, Food Stamp, and Medi–Cal programs as well as the annual costs for the automation systems supporting these programs. These costs combined exceed $3.6 billion in total funds and nearly $1.5 billion from the General Fund.
Figure 4
Costs of Eligibility and Enrollment Systems
2009–10 (In Millions)
|
|
General Fund
|
Federal Fundsa
|
County Funds
|
Total Funds
|
|
County Administration Costs
|
|
|
|
|
|
CalWORKs
|
$223
|
$356
|
$8
|
$587
|
|
Food Stamp
|
438
|
627
|
166
|
1,231
|
|
Medi–Cal
|
745
|
838
|
—
|
1,583
|
|
Totals
|
$1,406
|
$1,821
|
$174
|
$3,401
|
|
Automation Systems Maintenance Costs
|
|
Four Consortiab
|
$80b
|
$64
|
$8
|
$152
|
|
MEDS (includes IEVS costs)
|
9
|
9
|
—
|
18
|
|
EBT
|
15
|
9
|
3
|
27
|
|
SFIS
|
8
|
3
|
—
|
12
|
|
Totals
|
$112
|
$85
|
$11
|
$209
|
|
Grand Totals
|
$1,518
|
$1,906
|
$185
|
$3,610
|
After adjusting for increased caseload and workload, county administration funding levels for the CalWORKs and Food Stamp programs have remained relatively flat over the last ten years. So–called “cost of doing business” increases for CalWORKs and Food Stamps have not been provided to counties in the annual budget process since 2001–02. However, cost of doing business increases for Medi–Cal administration were provided through 2007–08. We note that counties have not received a cost of doing business increase in Medi–Cal since 2007–08.
Given the current magnitude and past growth in these costs, it is appropriate, in our view, that the Legislature take steps to ensure that administrative costs for these programs are contained or reduced where possible while maintaining an eligibility determination process that is accurate and timely.
Assumptions of Administrative Savings Seem Overstated
Our analysis indicates that the level of annual ongoing administrative savings assumed by the Governor is most likely significantly overstated. First, the administration’s estimate does not take into account the initial development costs for a new system. These costs would likely be in the hundreds of millions of dollars. Second, the level of administrative savings that has been suggested appears to be unrealistic. The $500 million estimate is the equivalent of about 34 percent of the current annual General Fund costs for county administration and maintenance of the related automation systems. The achievement of such savings would mean deep reductions in county administration staffing as well as in the costs of automation systems. The administration has not yet provided us justification of how automation changes would allow for savings of this magnitude.
Our analysis does indicate, however, that a lesser but still meaningful level of savings could be achieved through the types of changes contemplated in Chapter 7. For example, our analysis indicates that substantial savings on future operations and maintenance costs eventually amounting to tens of millions of dollars and potentially up to the low hundreds of millions of dollars annually could be generated by consolidating numerous consortia systems into fewer systems. In addition, efficiencies could result from implementation of the various back–end improvements described earlier in this report that would reduce the administrative burden on county eligibility workers and reduce the overall number of staff needed to perform eligibility and enrollment functions.
However, absent the development of a specific plan to improve eligibility and enrollment systems—the plan that the administration is still developing—it is difficult to assess ultimately what specific level of savings might be achieved through such changes.
Changes Likely to Increase Benefit Costs
If the Legislature takes steps to improve beneficiary access to the target programs and to simplify the enrollment and eligibility determination processes—the so–called front–end improvements discussed above—it is likely that there will be increased caseloads and related state benefit costs in these programs. Our analysis indicates that the increase in benefit costs may exceed the anticipated administrative savings from such changes.
Any steps the Legislature takes to make it easier for potential beneficiaries to apply for the three target programs are likely to ultimately increase the number of persons enrolled in these programs. Due to the significant cost of benefits in both the CalWORKs and Medi–Cal programs, even minor increases in caseload are likely to result in significant increases in the state cost of program benefits and administration. Figure 5 shows our estimates of the cost of potential increases in caseload and the related General Fund increase in benefit costs for the three target programs. The figure also shows how these increases in costs erode, and in some scenarios, far exceed, the maximum estimated level of savings proposed by the Governor.
Figure 5
Benefit Costs Could Exceed Administrative Savings
(In Millions)
|
General Fund Cost
|
Percent Increase in Caseload
|
|
1
|
2
|
3
|
4
|
5
|
|
CalWORKs benefits
|
$35
|
$70
|
$105
|
$140
|
$175
|
|
Food Stamp benefitsa
|
—
|
1
|
1
|
2
|
2
|
|
Medi–Cal benefitsb
|
169
|
337
|
506
|
675
|
844
|
|
Total Increased Costs
|
$204
|
$408
|
$612
|
$817
|
$1,021
|
|
Governor’s assumed savings
|
–$500
|
–$500
|
–$500
|
–$500
|
–$500
|
|
Net Savings (–)/Costs
|
–$296
|
–$92
|
$112
|
$317
|
$521
|
Given that the number of uninsured persons who are eligible for but not enrolled in Medi–Cal alone is at least 500,000, a caseload increase of at least 1 percent (73,000 individuals) or more due to front–end improvements would not be unreasonable. We estimate that if caseloads experienced greater than a 2 percent increase in growth from such front–end changes, the resulting impact would be a net increase in state costs even if one assumes that a full $500 million in administrative savings can be achieved. Finally, in addition to the increase in program benefit costs that is shown in Figure 5, the state also would experience some marginal increase in the costs of administering these programs because of the increased caseload, such as for any additional welfare program staff needed to complete additional eligibility determinations.
Changes Could Have Other Fiscal and Policy Benefits
From a broader perspective, the types of changes contemplated under Chapter 7, primarily those so–called front–end improvements, may improve the quality of care and assistance provided by the target programs and result in other fiscal and policy benefits. For example, these changes are likely to make it easier for people who are statutorily eligible for these programs to begin receiving benefits. Also, such an expansion of state programs may reduce the burden on counties providing services to low–income individuals. Moreover, eligibility simplifications could reduce “churning” or individuals and families moving on and off the caseloads of these programs. Some studies have found, for example, that churning disrupts care and adds to the administrative cost of processing and reprocessing children who are eligible for Medi–Cal.
Thinking Through Consortia Strategies
As it considers making significant changes to eligibility and enrollment processes for its major health and social services programs, the Legislature faces some key decisions regarding the future of the consortia systems soon. These include decisions about whether to launch a project to replace the Los Angeles County consortium and about how many consortia the state will support in the future.
LEADER Replacement System
As noted above, LEADER is one of the four consortia systems. It is currently near the end of a procurement for a replacement system. The Legislature originally approved a new LEADER replacement system in the 2007–08 Budget Act after Los Angeles County declared that the existing systems would not meet their program and business needs. However, in the 2009–10 Budget Act, the Legislature delayed the LEADER replacement project by six months (from January 2010 to July 2010) due to the state’s financial condition. The 2010–11 Governor’s Budget proposes delaying the project another six months to further defer costs. Currently, project managers plan to contract with a vendor in January 2011.
To date, $5 million (all funds) has been spent on planning and procurement activities for the LEADER replacement project. The project is estimated to cost $530 million (all funds) over five years.
New LEADER System Costs Will Be Significant. Currently, the project is in the relatively early planning stages. However, once the selected vendor begins building the system in early 2011, there will be significant costs, beginning with $50 million, all funds, in the first year of development followed by four years at about $100 million each. Once the system is completed, annual maintenance costs are estimated to be about $70 million, all funds.
LEADER and Chapter 7. Since approving a LEADER replacement system, the Legislature enacted Chapter 7, which establishes a new state goal of minimizing the number of technology systems the state operates for the delivery of health and social service programs. The enactment of this new legislative policy, along with the proposed price tag for a new LEADER system, raises the question as to whether work should continue to move forward on a LEADER replacement system, or whether Los Angeles County’s automation needs should be addressed as part of a more comprehensive, long–term statewide project to transform the state’s eligibility and enrollment systems.
The Legislature could go forward with the LEADER replacement project with the intent that that system would become the technological platform to which one or both of the other consortia systems migrate in the future. This would pave the way for the state to reduce the number of consortia systems in the future. (We discuss the pros and cons of having fewer consortia systems below.) The Legislature would need to ensure that the new system is adaptable enough to eventually handle statewide needs and requirements for multiple programs and counties.
How Many Consortia Systems?
The decision on whether to proceed with LEADER is really part of a larger and even more complex set of policy choices that are before the Legislature—determining the appropriate number of consortia systems that the state ultimately should support. As noted above, Chapter 7 directs the administration to minimize the number of technology systems involved in performing the eligibility determination process. By June 2010, after the ISAWS counties migrate to the C–IV system, there will be three consortia systems, instead of the current four. Is this the optimal number of systems or should there be an attempt to reduce this further? What are the merits and challenges to having two or even a single statewide system? Below, we present some of the advantages and disadvantages of having three, two, and a single statewide system.
Three Systems. Three consortia systems represent the status quo. The advantage here is that business could go on as usual in most counties. County staff would continue to use the systems that were tailored for their business practices. There would also be no large–scale transition to another system, and less possibility of disruption to services for recipients. Additionally, having three systems encourages competition and innovation among the consortia. For example, efforts by C–IV to develop an online portal spurred subsequent efforts to improve CalWIN.
The disadvantages of retaining three systems are that the state would continue to pay for the maintenance and operation of each as well as for separate procurements every time a system’s vendor contract expired and/or new systems needed to be developed. In addition to these costs, the continuation of three systems would not address the lack of standardization in California’s welfare operations nor improve communication between consortia counties—both important factors if the goals set forth in Chapter 7 are to be achieved.
Two Systems. Consolidation of three systems into two would begin to address some of the issues mentioned above. In our Analysis of the 2008–09 Budget Bill, we recommended such an approach on the basis that it would reduce system maintenance and support costs as well as avoid future development costs for new systems. Additionally, with two systems, the state could begin to further standardize its health and social services operations.
However, such a consolidation does have some significant drawbacks. Some counties would have to adapt to a new IT system and to new business practices that go along with that system. Moreover, if such a transition moved forward without county buy–in and cooperation, there is the risk that county workers would fail to fully utilize the new system, leading to short–run inefficiencies in administering programs and potential disruption of services and benefits.
A Single Statewide System. Further consolidation to one system would in theory allow the state to leverage its buying power and save the most money on consortia development and operations in the long–term. The state would only have to pay for maintaining, operating, and supporting one system. There would also be easy communication within and among counties and one set of business practices for the entire state. Additionally, a single statewide system might reduce the need for the state to operate so many of the ancillary automation systems described above (such as WDTIP, SFIS, and MEDS). If successfully implemented, this approach could ultimately take the state furthest toward the goals outlined in Chapter 7.
However, moving to a single statewide system would be difficult for the state to accomplish. It would likely not be flexible enough to meet the individual programmatic needs of each county, thus making it harder to get county buy–in to carry out such a major change. Also, there are inherent risks in attempting to build or upgrade to a single statewide system, as the state realized after tackling a single child support system. Such a system would be large and complex, take years to design and build, and would likely cost more than originally estimated.
Lastly, there is a question of governance of such a new system. Currently, vendor and county staff are responsible for their respective consortia. Under a single system, it is unclear who should be responsible for maintenance of the system—the state, a private vendor, or some representative group of counties. These implementation issues would have to be carefully considered if the state were to move to a single system.
Creating Buy–In
As directed under Chapter 7, HHSA began in December 2009 to conduct a series of stakeholder meetings to help launch efforts to reform the administration of CalWORKs, Food Stamp, and Medi–Cal eligibility and enrollment processes. From the outset, these meetings have been contentious, partly a result of disagreements among stakeholders trying to resolve and prioritize the goals set forth in Chapter 7.
Involvement of stakeholders is important in this process, but none more so than counties. Counties have been and are likely to continue to be an important partner in the state’s administration of the CalWORKs, Food Stamp, and Medi–Cal programs. This is in large part because of the history of the administration of these programs, the complexity of administering these programs across a state with both a large population and geographic size, and due to the current reliance of these programs on the county workforce. In order to move forward and achieve the outcomes identified in Chapter 7, we believe the Legislature will need to find ways to diffuse these conflicts and retain counties as a valuable planning partner in this endeavor.
One possible approach would be to create incentives for counties to identify and implement strategies that would improve the efficiency of county administration of these programs. For example, the Legislature could enhance the county share of any cost savings generated by reforming the eligibility and enrollment determination process based on objective measures of county performance. Absent such incentives, counties may lack sufficient motivation to undertake the sometimes–difficult changes needed to achieve efficiencies in the system. Their full engagement in this process is important if significant investments by the state in new systems are to produce worthwhile results.
Inherent in the state providing funding to counties for the administration of eligibility determinations for these programs is that counties are paid to provide a certain level of service that ensures timely and accurate eligibility determinations. However, the state has not consistently measured county performance and how service levels have or have not changed over time as the levels of funding provided by the state have fluctuated. As part of improving counties’ efficiency, the state could develop metrics to establish a service level and a process for tracking over time changes in the funding provided and the service levels delivered. The county incentive structure proposed above could also address this issue.
A Roadmap for the Legislature
Improving the eligibility determination and enrollment processes for CalWORKs, Food Stamp, and Medi–Cal, and possibly other health and social services programs, presents an opportunity for the Legislature to reduce the cost of administering these programs as well as improving access to these programs for beneficiaries. However, as our fiscal analysis above indicates, a modest 2 percent increase in enrollment in these programs as a result of an improved enrollment process could result in additional state costs in excess of the likely administrative savings from such changes. Given the state’s current difficult fiscal condition, this is a challenging time to begin to implement changes that would ultimately increase state costs at the very time the Legislature must consider proposals that would drastically reduce or eliminate some of these same programs in order to balance the state’s budget.
As the administration continues its stakeholder process to develop a plan to implement Chapter 7, we recommend a general approach that the Legislature may wish to consider to navigate these difficult choices.
Prioritize Changes That Improve County Efficiency. We recommend that the Legislature direct the state departments that will be responsible for development of new eligibility and enrollment systems, in conjunction with HHSA, to work collaboratively with counties to prioritize some of the back–end improvements that would increase the efficiency of counties’ administration of the eligibility processes for these programs. One such example would be the development of new systems to share eligibility–related documentation electronically throughout the state and among programs. The advantages and disadvantages of this and other best practices should be vetted during the stakeholder process to assess which have the greatest potential to increase the efficiency of county administration of eligibility determination.
Assess Requirements of Federal Health Reform. The Legislature should direct HHSA and related health programs to assess the requirements of federal health care reform on the state‘s eligibility and enrollment determination processes. It is likely that the state will gain a better understanding of these requirements as the federal government releases regulations to implement the new federal law. At a minimum, it is clear that federal reform will require changes to the current eligibility and enrollment process for Medi–Cal and other health programs. It is also possible that the state will be required to invest in the development of new IT systems to comply with federal requirements.
Provide a Fiscal Incentive for County Cooperation. The Legislature should consider a strategy for sharing cost savings with counties to help ensure county buy–in for the successful implementation of improvements in eligibility and enrollment processes called for under Chapter 7. This approach would reward counties that implemented changes that resulted in administrative savings in these programs based upon objective measures of county performance. These types of changes would probably require legislation.
Be Aware That Certain Improvement Are Likely to Increase Caseload and Costs. An increase in enrollment in Medi–Cal and CalWORKs will result in increased state benefit costs, which, given the state’s fiscal condition, may not be in the state’s best interest at this time. Accordingly, we recommend that the Legislature require the departments to conduct a cost–benefit analysis of the impact of implementing various front–end strategies, such as enabling applicants to apply online to determine the likely impact of each such change on caseload and related costs.
Build in Flexibility for Future Improvements. In the future, once the state’s fiscal condition has improved, the Legislature may wish to consider undertaking reforms to the eligibility determination processes and making other significant changes that would improve access by eligible applicants for these programs. For this reason, we recommend that any new eligibility and enrollment systems be developed with the flexibility to incorporate such changes in the future. For example, these systems should be flexible enough to easily allow future implementation of online program applications by individuals for the multiple health and social services programs for which they may be eligible. Any new systems should also be designed so that, in the future, they could interface with other databases to verify documents submitted by applicants for their eligibility.
Consider the Future of the Consortia Systems. As the Legislature considers how best to move forward with Chapter 7 to improve the eligibility and determination processes and systems for health and social services programs, it should concurrently be considering the future of the consortia. In our Analysis of the 2008–09 Budget Bill (please see
page C–158), we concluded that a reduction in the number of consortia to two systems would reduce system maintenance and support costs as well as avoid future development and procurement costs for new systems. This would also be consistent with the Legislature’s stated intentions in Chapter 7 to move toward fewer technology systems for health and social services programs. We continue to see two or fewer systems as an advantage to the state. In addition to savings and cost avoidance, fewer systems would allow the state to begin standardizing its welfare operations at the county level.
We recommend that the Legislature continue to take steps to reduce the number of consortia systems over time. We see two possible routes to two systems, as we mentioned above. Migrating Los Angeles County to an existing consortia would be the quickest route to two systems. The second, longer–term route would be to build the new LEADER system but to require the CalWIN and/or C–IV counties to migrate when their respective systems become obsolete. Should the Legislature decide to pursue the second option and proceed with LEADER development, it should first ensure that the new LEADER replacement system would be flexible enough to allow the other systems to seamlessly work and communicate among one another and allow for a relatively easy consolidation of counties in the future. We believe both routes have merit and that the Legislature should choose one of these two routes.