Earlier this year, California submitted a proposal to renew its Section 1115 waiver, which is due to expire at the end of October. The state is currently negotiating with the federal government over the terms and conditions of this waiver renewal. In this post, we examine key issues and concerns related to the availability of federal funding for California’s proposal. The post provides a primer on how Section 1115 waivers are generally financed, an overview of California’s proposal, and a discussion of the challenges the proposal faces within that financing structure.
LAO Contacts: Felix Su and Amber Didier
October 13, 2015
Section 1115 Waiver Renewal:
Key Medi-Cal Financing Issues Remain Outstanding
Introduction
The federal government grants states flexibility in administering their Medicaid programs (called Medi-Cal in California) through “waivers,” such as those allowed under Section 1115 of the federal Social Security Act. When a state’s waiver request is approved by the federal government, the state is permitted to waive certain federal requirements on the basis that the waiver serves to further the purpose of the state’s Medicaid program. (For general background on Section 1115 waivers, see this publication by the Kaiser Family Foundation.)
California’s current Section 1115 waiver, known as the “Bridge to Reform,” is set to expire on October 31, 2015. (For an overview of the Bridge to Reform, see this publication by the California HealthCare Foundation.) In late March, the Department of Health Care Services (DHCS) submitted a concept paper for a renewal of the Section 1115 waiver to the federal Centers for Medicare and Medicaid Services (CMS). The proposal, titled “Medi-Cal 2020,” asks the federal government to renew the waiver for another five years and to provide over $17 billion in additional funding to California to finance new demonstration projects that would otherwise be ineligible for federal Medicaid reimbursement.
At the time of this post, DHCS is still negotiating with CMS over the terms and conditions for Medi-Cal 2020. Issues surrounding federal financing are at the fore of these negotiations. As the renewal deadline approaches, having an informed expectation about the size and scope of Medi-Cal 2020—as well as the prospects for individual projects included in the state’s application—requires a working knowledge of these financing issues. This post aims to provide that knowledge—first with a primer on how Section 1115 waivers are generally financed, next with an overview of California’s proposal, and lastly with a discussion of the challenges the proposal faces within that financing structure.
How Are Section 1115 Waivers Financed?
Budget Neutrality
There are no federal statutory or regulatory restrictions on federal spending under Section 1115 waivers. However, it is CMS’s longstanding policy that—as a condition for receiving approval—states must demonstrate their proposed waivers would be “budget neutral” to the federal government. This means total federal costs for a state operating a waiver cannot exceed total federal Medicaid spending in the state absent the waiver.
Ceiling. Each state submits a budget neutrality calculation as part of its waiver application. The calculation separately projects federal spending under two scenarios: with and without the proposed waiver. Once approved by CMS, the “without-waiver” projection serves as a ceiling on the total amount of federal funding potentially available over the life of the waiver. (For general information about the process for calculating budget neutrality, see this report by the Government Accountability Office [GAO].)
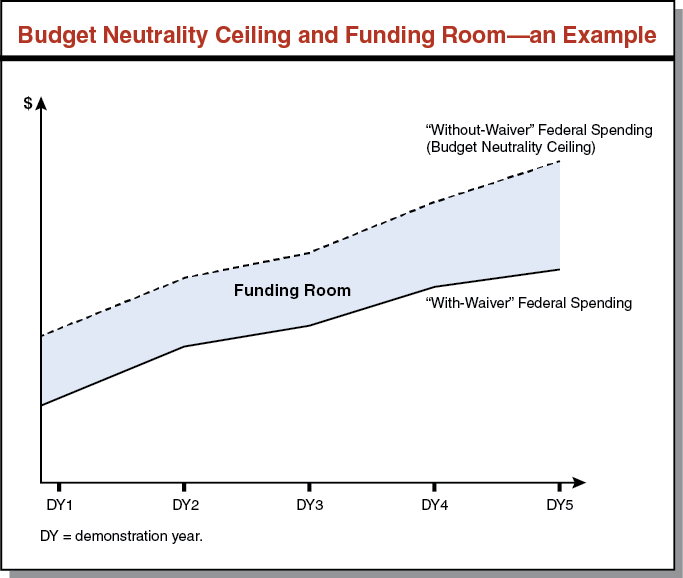
Funding Room. To satisfy budget neutrality and finance new federal spending, a Section 1115 waiver must (1) achieve federal savings that are not fully offset by new waiver spending and/or (2) redirect existing federal funding to finance this new spending. In the first case, the savings attributed to the waiver create “room” under the budget neutrality ceiling for additional federal funding. This is illustrated conceptually in the figure below.
Nonfederal Matching Requirement
Generally, Section 1115 waivers permit states to receive federal matching funds for expenditures that are not otherwise allowable under the Medicaid statute. Standard Medicaid funding rules—which require states to pay the nonfederal share of costs at applicable matching rates, using appropriate state and local funding sources—usually apply to waiver expenditures.
What Is California Proposing for Medi-Cal 2020?
The DHCS’s concept paper contains detailed descriptions of the various demonstration projects proposed for Medi-Cal 2020. Below, we briefly summarize the major projects proposed in the waiver, and provide the additional five-year federal funding amount associated with each project. None of the projects would involve state spending through a General Fund match. Instead, counties and other local governments would provide the nonfederal share through certain expenditures and funding transfers. For the last set of projects, the state has asked CMS to waive the nonfederal matching requirement altogether. (We return to this point when we discuss the state’s proposed waiver financing in the next section.)
Global Budget for Uninsured ($1.2 Billion). Within the regular Medicaid program, the federal government provides each state an annual allotment of Disproportionate Share Hospital (DSH) funding. (For general background on DSH payments, see this report by the Congressional Research Service.) California’s DSH allotment is available to public hospitals operated by counties and the University of California—known collectively as designated public hospitals (DPHs)—to help defray their costs of uncompensated care for Medi-Cal and uninsured patients. Under the Bridge to Reform, the federal government provides additional uncompensated care funding through the Safety Net Care Pool (SNCP). This includes annual capped payments to DPHs for uninsured costs that are not covered by DSH funding.
For Medi-Cal 2020, the state has requested CMS to maintain $236 million in annual SNCP uncompensated care payments to DPHs. Moreover, the state seeks to combine this continued SNCP funding with its existing DSH allotment to create a “global budget” payment system for DPHs. The goal is to move away from the current cost-based method of distributing uncompensated care payments, and instead grant DPHs more flexibility in using these funds to provide better-coordinated care for the uninsured. (The DSH portion of the global budget proposal—which amounts to $5 billion over the life of the waiver—represents redirected as opposed to new funding, since DSH funding is available without a waiver.)
Offsets for State Health Programs ($2 Billion). The SNCP for the Bridge to Reform also provides up to $400 million annually in federal funding to offset General Fund costs in certain state health programs, such as the Breast and Cervical Cancer Treatment Program, California Children’s Services, and the AIDS Drug Assistance Program. The state has asked CMS to extend this amount of annual funding as part of Medi-Cal 2020.
Public Hospital Incentive Program ($4 Billion). The Bridge to Reform provides annual incentive payments to DPHs for undertaking projects related to infrastructure development and patient care improvement. The state has proposed a $4 billion “successor” incentive program over the life of the waiver to support additional public hospital projects under Medi-Cal 2020. (The program would be widened to include hospitals operated by municipalities and health care districts.)
Reinvestment Projects ($10 Billion). Finally, the state has proposed so-called “reinvestment” projects that would be funded entirely with federal funding. These projects represent major innovations unique to Medi-Cal 2020 and fall under five main categories: supportive housing, workforce development, managed care incentives, fee-for-service (FFS) incentives, and whole-person care pilots. While DHCS is requesting $10 billion cumulatively in reinvestment project funding over the life of the waiver, it does not specify how this amount would be allocated across the different project groups.
Where Would California’s Requested Funding Come From?
In late January, DHCS held a detailed presentation on the state’s request for funding and proposed financing mechanisms for Medi-Cal 2020. (A recording is available on DHCS’s website.) Here, we highlight key takeaways from the presentation.
Calculating Spending Limits and Funding Room
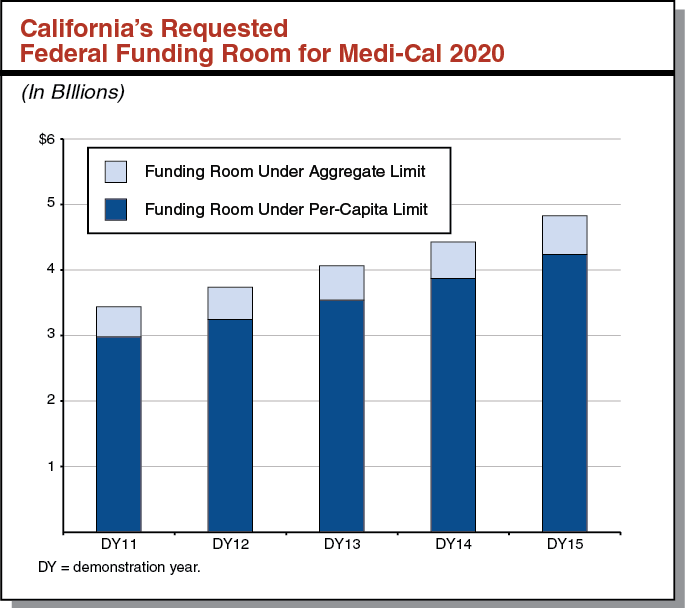
California’s budget neutrality ceiling for the Bridge to Reform consists of two parts. The first is a per-capita limit on federal spending for Medi-Cal enrollees. The second is an aggregate limit related to Medi-Cal FFS expenditures on DPHs. The two limits combined form the total “without-waiver” ceiling for the Bridge to Reform. The difference between this total ceiling and the state’s “with-waiver” spending projection creates room for additional federal funding under the waiver. California has asked CMS to maintain this two-part ceiling as the basis for determining potential funding under Medi-Cal 2020. The figure below shows the requested funding room under each proposed spending limit in the state’s application. Next, we describe the methods and assumptions proposed by DHCS to justify this level of funding to CMS.
Room Under FFS Per-Capita Limit. Some states, including California, have recently incorporated their Medicaid managed programs into their Section 1115 waivers. (It is possible for a state to operate a Medicaid managed care program without a Section 1115 waiver, as described on CMS’s website.) Up to now, this has allowed states to develop “without-waiver” per-capita spending projections that assume all Medicaid enrollees receive services through FFS. In determining the budget neutrality ceiling, this “without-waiver” scenario is compared to a “with-waiver” scenario that takes into account Medicaid managed care. The hypothetical FFS “without-waiver” scenario typically grants states a high budget neutrality ceiling, as well as a large degree of funding room under that ceiling. This occurs because states’ projections assume that FFS per-capita spending would be higher—and grow much faster—than managed care per-capita spending assumed under the “with-waiver” projections.
In 2010, California took this approach by consolidating federal authority for its various managed care models under the Bridge to Reform. Because Medi-Cal enrollment has been predominantly managed care for the past several years, California’s “without-waiver” projection uses historical FFS cost trends that predate 2010. California’s “with-waiver” calculation is initially a projection based on more recent managed care cost trends. The state is required to update the “with-waiver” calculation to reflect actual managed care spending as it occurs throughout the life of the waiver.
The vast bulk of funding room for the Bridge to Reform comes from the difference between the FFS “with-waiver” projection and the managed care “without-waiver” calculation. California has asked to continue receiving “credit” for managed care savings in Medi-Cal 2020, by again basing its “without-waiver” ceiling on a FFS scenario. This assumption accounts for nearly $18 billion of the $20.5 billion in funding room that the state claims should be available for Medi-Cal 2020. (Again, the state has asked CMS to spend over $17 billion of the assumed $20.5 billion in funding room on waiver-related projects.)
Room Under DPH Aggregate Limit. Under the Bridge to Reform, Medi-Cal makes FFS payments for inpatient care at DPHs based on the hospitals’ reportable costs. To be eligible for federal reimbursement, the total amount of Medicaid FFS payments to hospitals within a state may not exceed a maximum amount known as the upper payment limit (UPL). In California, the UPL for hospital services has historically been 5 percent to 10 percent above hospitals’ reportable costs. Consistent with the Bridge to Reform waiver, the state’s “without-waiver” projection for Medi-Cal 2020 assumes DPHs are paid at the UPL. The state’s “with-waiver” projection assumes the hospitals’ reportable costs and therefore the associated payments remain below the UPL, thereby creating an additional $2.6 billion in funding room under budget neutrality.
Federal “Shared Savings” for Reinvestment Projects
To pay for the five groups of reinvestment projects, the state has asked CMS to make $10 billion available—without the normally required nonfederal match—by “sharing” a portion of the federal funding room that remains after accounting for the rest of the proposed waiver spending. The figure below shows this “shared savings” calculation. After “reinvesting” an additional $10 billion in California, the federal government would still be left with over $3 billion in “savings,” as compared to the budget neutrality ceiling proposed by the state.
California’s Proposed “Shared Savings” Calculation for Medi–Cal 2020
Federal Funding Room and Expendituresa, (In Billions)
|
Proposed per–capita savings (managed care versus FFS) |
$17.9 |
||
|
Proposed public hospital FFS savings (cost–based versus UPL) |
2.6 |
||
|
Total Funding Room Under Proposed Budget Neutrality Ceiling |
$20.5 |
||
|
Less: |
|||
|
SNCP—uncompensated care payments for global budget for uninsured |
($1.2) |
||
|
SNCP—General Fund offset for state health programs |
(2.0) |
||
|
Public hospital incentive program |
(4.0) |
($7.2) |
|
|
Remaining Funding Room Before “Shared Savings”/Reinvestment Programs |
$13.3 |
||
|
Less: |
|||
|
Reinvestment programsb |
($10.0) |
||
|
Final Federal Savings Under State’s Waiver Proposal |
$3.3 |
||
|
a Amounts in parentheses denote federal expenditures. b Under the state’s proposal, reinvestment programs would be funded from federal “shared savings” without a nonfederal match. FFS = fee–for–service; SNCP = Safety Net Care Pool; and UPL = upper payment limit. |
|||
What Are Financing Challenges Faced by California’s Proposal?
Funding Room May Shrink Drastically
CMS May Require State to Rebase “Without-Waiver” Projection to Managed Care… At a mid-July stakeholder meeting, DHCS officials stated they “have been concerned about CMS discussions of rebasing away from the FFS calculations on the ‘without-waiver’ side for California.” In other words, CMS may require California to use a starting baseline of more recent per-capita costs in managed care and/or project those costs forward using growth rates based on managed care. According to DHCS, CMS intends to issue a “national policy” on budget neutrality for states like California with longstanding Medicaid managed care programs. We note the GAO report criticized CMS for inconsistently permitting certain states to (1) include hypothetical costs in their “without-waiver” baselines and (2) use outdated expenditure data and growth rates for their projections. Both criticisms could be seen as applying to California’s budget neutrality calculation, although the GAO report did not specifically mention CMS’s treatment of the Bridge to Reform.
…Which Could Wipe Out Most of State’s Budget Neutrality Funding Room. In the extreme scenario, forcing California to rebase its spending baseline and growth rates to managed care could result in identical per-capita spending projections with and without the waiver. Zero difference between these projections would translates into zero savings—and funding room—from placing managed care under the Section 1115 waiver. As noted by DHCS, “this could mean [California has] no savings/budget neutrality to implement program changes.” The remaining $2.6 billion in funding room from the DPH limit cannot support the full SNCP extension proposed by the state. $2.6 billion is also insufficient to fund the public hospital incentive program at the level proposed by the state. While DHCS has reported that “CMS continues to say they want to rebase, but that it is not their intention to zero out savings,” it is unclear how this type of rebasing would not lead to a significant decrease in allowable funding room under the waiver.
Restrictions on Accessing and Using Funds
Even if California were able to preserve most of its proposed funding room under the per-capita spending limit, it faces two additional hurdles—one certain, the other likely—to using the funding as originally envisioned in the concept paper.
CMS Has Rejected “Shared Savings” Mechanism. In a September written update, DHCS acknowledged that after further discussion, “[DHCS and CMS] agree that the legal barriers to [the state’s] proposal to earn nonfederal share credit…cannot be overcome, and [DHCS] agreed to identify and use other sources of nonfederal share to fund as much as possible [of the proposed reinvestment projects].” However, DHCS’s concept paper originally claimed that “absent this shared savings approach, California would be extremely limited in its ability to enact the proposed…programs.” This implies that for at least some expenditures related to the reinvestment projects, it could be difficult for the state to furnish a suitable nonfederal match.
CMS May Cease Funding SNCP. At the July stakeholder meeting, DHCS indicated “there will also be a new national policy on uncompensated care pools” like California’s SNCP. While the details of this policy are still unknown, it could place at risk $236 million annually in the global budget for the uninsured and $400 million annually in General Fund offsets for state health programs. According to DHCS, CMS has expressed general reluctance to continue defraying states’ uninsured costs beyond DSH. This may in part be due to states’ option to expand Medicaid under the Affordable Care Act. Although DHCS requested CMS to extend the $400 million in offsets for state health programs, the 2015-16 Budget Act does not assume the offsets will continue, and backfills their presumed loss with General Fund.
Conclusion
In practice, CMS policy and discretion over waiver funding are highly subjective, yet sometimes influenced by external pressures like the GAO report. The final agreement for Medi-Cal 2020—which depends heavily on CMS’s decisions about what it is able and willing to approve—will spell out (1) how much additional federal funding is potentially available to California over the next five years, (2) what the state must do to access that funding, and (3) which projects may be supported with the funding. While many stakeholders have focused their interest in the third component, it is ultimately contingent on the first two. We will monitor further developments as the waiver renewal is finalized and provide updates as appropriate.
