LAO Contact
May 16, 2019
The 2019-20 May Revision
Analysis of the Governor’s January and May Mental Health Workforce Proposals
Summary
January Budget Proposed $50 Million in One-Time General Fund for Mental Health Workforce. To ameliorate what the Governor considers to be statewide and regional shortages of mental health professionals, the Governor’s January budget proposed a $50 million one-time General Fund augmentation for existing state programs that provide scholarships and student loan repayment for mental health professionals who agree to work in underserved areas.
May Revision Proposes Additional State Funding for Mental Health Workforce. The May Revision proposes allocating $100 million in state Mental Health Services Act (MHSA) revenues to fund the 2020‑25 mental health Workforce Education and Training (WET) Five-Year Plan. The 2020‑25 WET Plan was released by the Office of Statewide Health Planning and Development (OSHPD) in February 2019, but until the May Revision did not come with any attached funding. Under the mental health WET program, the state has historically funded a variety of programs and strategies to improve the supply and distribution of the state’s mental health workforce. These programs and strategies include, for example, scholarships, student loan repayment, psychiatric residencies, psychiatric fellowships, and clinical rotations. While the $50 million in General Fund proposed in January would largely only support the scholarship and student loan repayments, it is our understanding that the Governor’s additional $100 million in MHSA funding would support all of the above strategies and others. As with the $50 million in General Fund proposed in January, the $100 million in funding would be available for expenditure through 2025‑26.
Mixed Evidence of Statewide Mental Health Workforce Shortages . . . Following a preliminary review of the state’s mental health workforce that we conducted earlier this year, we find mixed evidence of a statewide shortage for mental health professionals overall. While certain mental health workforce projections show the state is likely to experience a shortage, other evidence we reviewed does not suggest this to be the case. That said, we find stronger evidence that the state could be experiencing a shortage of psychiatrists.
. . . But Regional Disparities in the Supply of Mental Health Professionals Exist. While the evidence is mixed regarding the presence of a statewide mental health workforce shortage, the evidence is strong that significant regional disparities exist in the supply of mental health professionals. Notably, regions such as the Inland Empire and the San Joaquin Valley have significantly fewer mental health professionals per capita than the state as a whole.
Uncertainty Around Whether Existing State Programs and Strategies Have Been Effective. Overall, existing state mental health workforce programs and strategies may have had some positive impact in increasing the overall number of mental health professionals throughout the state. However, our preliminary review of mental health workforce data showed little relationship between the regions of the state experiencing the greatest workforce challenges and the work locations of former program beneficiaries.
Options for Legislative Consideration
We provide several options for the Legislature to consider as it evaluates the Governor’s proposals.
-
Take Pause to Identify the State’s Needs and the Most Cost-Effective Strategies. Under the Governor’s May Revision, the state would provide $150 million in 2019‑20 for mental health workforce development, prior to necessarily having identified the state’s most critical mental health workforce needs and the most cost-effective strategies for ameliorating them. Accordingly, the Legislature could consider taking pause and formulating a more comprehensive long-term strategy on mental health workforce. Exercising this first option would involve delaying funding until many of the outstanding uncertainties related to the state’s mental health workforce strategies are better understood.
-
Scale Back Funding. Historically, what otherwise would have been local MHSA funding for counties was redirected to fund state mental health WET programs. Under the Governor’s proposal, however, only funding designated for state purposes (General Fund and the portion of MHSA funding dedicated to state activities and programs) would support state mental health workforce programs. The Legislature could consider reducing the amount of state funding provided for mental health workforce programs and instead either allow (as currently) or require a financial contribution from counties to fund local workforce programs. (We would note that, under the MHSA, counties receive ongoing, flexible funding from the state that may be used—at counties’ discretion—for workforce programs.)
-
Establish Parameters for How Funding Is Allocated. Another option is to approve the Governor’s proposal, but add parameters to ensure the funding is targeted toward the areas of greatest need. For example, funding could be prioritized toward regions of the state—such as the Inland Empire and the San Joaquin Valley—that are likely experiencing the most acute mental health workforce shortages. In addition or alternatively, the Legislature could target the funding toward those mental health professions for which there is the greatest evidence of shortages, such as psychiatrists.
Provide Flexible Funding to High-Need Counties. The Legislature could consider redirecting all or a portion of the funding proposed by the Governor to instead provide flexible funding to counties facing the most acute workforce challenges, which these counties could use in accordance with local needs and conditions. For example, counties could choose to use such funding to support local education and training programs, student loan repayments, or improve pay in areas where they are facing acute recruiting challenges.
Introduction
In January, the Governor proposed a $50 million one-time General Fund augmentation for existing mental health workforce programs that are administered by OSHPD. In the May Revision, the Governor proposes an additional $100 million in MHSA funding for mental health workforce. This post (1) provides background on the state’s mental health workforce, (2) gives an overview of existing programs and funding aimed at improving the state’s mental health workforce, (3) summarizes and assesses the Governor’s proposals, and (4) provides options for legislative consideration.
Background
In this section, we provide a brief overview of public community mental health services delivery and funding in California. We then provide background on the various professions that provide mental health services. Finally, we briefly summarize the history of mental health workforce funding in the state.
Community Mental Health Services
Defining Community Mental Health. Mental health services include the diagnosis and treatment for individuals experiencing mental illness. Common mental health diagnoses include depression and schizophrenia. Common treatments include therapy, crisis intervention and stabilization, medication, and inpatient psychiatric services. As used in this post, “community mental health services” generally comprise all mental health services delivered in community settings, thereby excluding those delivered in certain other settings, notably correctional settings. Community mental health services are commonly paid for by both private and public health insurance. According to 2015 national estimates, private sources—such as commercial health insurance and out-of-pocket expenditures—paid for about one-third of mental health services. Medicaid accounts for another one-third of spending and Medicare and other public sources comprise the remaining one-third.
In California, Public Community Mental Health Services Are Primarily Delivered and Funded Through Counties. In California, counties play a major role in the funding and delivery of public mental health services. In particular, counties are generally responsible for arranging and paying for community mental health services for low-income individuals with the highest mental health needs. Counties deliver these services through a mix of county mental health staff and contracted providers. In 2018‑19, counties are receiving $9.3 billion in funding for community mental health services. About half of funding for county mental health services is provided by the state through block grants that grow on an annual basis in line with state tax revenues. Federal Medicaid funding makes up most of the remaining funding.
Recent Policy Changes Have Likely Led to an Increase in Demand for Mental Health Services and Providers. Demand for community mental health services has very likely increased over the last several years, in large part due to the federal Patient Protection and Affordable Care Act (ACA), implemented in 2014. Under the ACA, California has experienced significant increases in the number of residents with health insurance, which has likely increased state residents’ willingness and capacity to seek mental health services. Funding for public community mental health services has also increased in recent years. Since the ACA was implemented, total annual funding for county mental health services has increased by 71 percent, from $5.5 billion to $9.3 billion.
Mental Health Professions
A Variety of Professions Provide Mental Health Services. In an effort to ensure quality care, state laws restrict the delivery of mental health services to licensed providers. Such licensure requirements generally impose minimum education and work-experience standards for providers to be allowed to practice independent of supervision. State law permits a variety of professions to deliver mental health services and establishes scope of practice rules for which types of services different professions may provide. For example, psychiatrists may prescribe medicine and provide a variety of diagnostic and therapeutic services. Psychologists, by contrast, may not prescribe medicine but may provide a similar array of diagnostic and therapeutic services as psychiatrists. Figure 1 summarizes the professions specializing in the delivery of mental health services.
Figure 1
A Variety of Professions Specialize in the Delivery of Mental Health Services
|
Profession |
Education Requirement |
|
Can Prescribe Medication |
|
|
Psychiatrist |
Medical degree |
|
Psychiatric nurse practitioner |
Master’s or doctorate |
|
Cannot Prescribe Medication |
|
|
Psychologist |
Professional doctorate |
|
Clinical counselor |
Master’s |
|
Clinical social worker |
Master’s |
|
Marriage and family therapist |
Master’s |
|
Psychiatric mental health registered nurse |
Master’s |
|
Psychiatric technician |
High school diploma |
Existing Mental Health Workforce Programs
State Administers a Variety of Mental Health Workforce Programs. Since even before the ACA, state policymakers have had concerns about the capacity of the state’s mental health workforce to meet demand for services. To address these concerns, the state and counties administer a variety of programs aimed at improving the overall supply, geographic distribution, and diversity of the state’s mental health workforce. Often, these existing programs offer (1) scholarships or stipends (as high as $25,000) for prospective mental health professionals still completing their education, (2) student loan repayment (as high as $105,000) for practicing mental health professionals, or (3) grants (as high as $1.6 million) that encourage the integration of psychiatric training programs into the public mental health system. In general, these existing programs are designed to support the workforce needs of the public community mental health system as well as some types of private providers that largely serve low-income populations.
State Programs Often Require Service Obligations in Exchange for Financial Assistance. The programs that provide scholarships, stipends, or student loan repayment include service obligations where recipients must work at an eligible location for a specified period of time—typically one-to-two years—or otherwise repay the scholarship, stipend, or loan repayment assistance. Eligible locations include practice sites located in designated shortage areas as well as certain safety-net clinics that serve low-income and other high-need populations, regardless of whether they are located in designated shortage areas.
OSHPD Is Responsible for Creating Five-Year Mental Health Workforce Plans. In addition to operating mental health workforce programs, OSHPD is responsible for developing five-year plans outlining strategies to meet the state’s mental health workforce education and training needs. These plans are known as “WET Five-Year Plans.” OSHPD’s most recent WET Five-Year plan was released in early 2019. As we describe in the next paragraph, historically, MHSA funding supported the funding priorities outlined in the previous WET plans. Under previous plans, the state funded a variety of mental health workforce development programs and strategies including, for example, scholarships, student loan repayment, psychiatric residencies, psychiatric fellowships, and clinical rotations.
Funding Specifically Dedicated to State Mental Health Workforce Programs Largely Expired in 2017‑18. The MHSA, approved by voters in 2004, places a 1 percent surtax on incomes over $1 million and dedicates the revenue to mental health services. A total of $445 million in MHSA revenues from the act’s initial years was set aside on a limited-term basis to fund state and county workforce initiatives outlined in previous WET plans. Roughly half of this funding was administered at the state level (most recently by OSHPD), with the other half going directly to counties to administer. The state and counties had through 2017‑18 to spend this $445 million. To continue funding into 2018‑19, the Legislature appropriated $11 million in one-time MHSA funding for state mental health workforce programs.
Counties Free to Dedicate up to 15 Percent of MHSA Revenue to Local Workforce Programs. The MHSA authorizes, but does not require, counties to spend a portion of their MHSA revenues on workforce development activities. The maximum amount of MHSA revenues that counties can spend on workforce development activities is around 15 percent of total MHSA revenues, though we would note that this 15 percent ceiling includes the total funding counties may dedicate to certain other purposes as well—namely to capital and technology acquisition and development and prudent reserves. Were counties to devote one-third of allowable MHSA funding to workforce programs, for example, almost $100 million annually in MHSA funding could be used. It is our understanding that counties have not generally chosen to devote significant MHSA funding to local mental health workforce development. In large part, this is likely due to the fact that the MHSA specifically dedicated a significant portion of MHSA revenues from the act’s early years to workforce development.
Governor’s Proposals
January Budget Proposed $50 Million in One-Time General Fund for Mental Health Workforce. To ameliorate what the Governor considers to be statewide and regional shortages of mental health professionals, the Governor’s January budget proposed a $50 million one-time General Fund augmentation for existing state programs that provide scholarships and student loan repayment for mental health professionals who agree to work in underserved areas.
May Revision Proposes Additional State Funding for Mental Health Workforce. The May Revision proposes allocating $100 million in state MHSA revenues to fund the 2020‑25 WET Five-Year Plan. The 2020‑25 WET Plan was released by OSHPD in February 2019, but until the May Revision did not come with any attached funding. While the $50 million in General Fund proposed in January would largely only support scholarship and student loan repayments, it is our understanding that the Governor’s additional $100 million in MHSA funding would support these as well as various other strategies that have been used historically to improve the supply and distribution of the state’s mental health workforce. A portion of the WET funding would support state mental health workforce programs, with the remaining funding going to regional partnerships (which generally employ similar approaches as the state to improve their local workforces). As with the $50 million in General Fund proposed in January, the $100 million in funding would be available for expenditure through 2025‑26. Figure 2 summarizes the key similarities and differences between the Governor’s January and May proposals, which we note are proposed to be implemented together (that is, the May proposal is in addition to the January proposal).
Figure 2
Similarities and Differences Between the Governor’s January and May Mental Health Workforce Proposals
|
January Proposal |
Additional May Proposala |
|
|
Funding |
||
|
Amount |
$50 million |
$100 million |
|
Fund source |
General Fund |
MHSF |
|
One time or ongoing |
One time |
One time |
|
Funding available for expenditure through 2025‑26 |
✔ |
✔ |
|
Delivery Systems |
||
|
Support the public mental health delivery system |
✔ |
✔ |
|
Support private mental health delivery systems |
✔ |
|
|
Administration |
||
|
Funds state programs administered by OSHPD |
✔ |
✔ |
|
Directly funds regional workforce partnerships |
✔ |
|
|
Strategies |
||
|
Student loan repayment |
✔ |
✔ |
|
Scholarships |
✔ |
✔ |
|
Educational stipends |
✔ |
|
|
Psychiatric residency program grants |
✔ |
|
|
Clinical rotations funding |
✔ |
|
|
Psychiatric fellowships for general practitioners |
✔ |
|
|
Peer personnel preparation |
✔ |
|
|
Outreach |
✔ |
|
|
Research and evaluation |
||
|
aProposal is in addition to, not in place of, the January proposal. MHSF = Mental Health Services Fund and OSHPD = Office of Statewide Health Planning and Development. |
||
Assessment
In this section, we provide our assessment of the magnitude and geographic distribution of potential mental health workforce shortages and the potential impact of the Governor’s proposals in ameliorating these potential shortages.
Mixed Evidence of Statewide Mental Health Workforce Shortages
Projections From Academic Researchers Predict the State Could Face a Shortage of Mental Health Professionals. Researchers at the University of California, San Francisco (UCSF) project that, unless the total number of people entering mental health professions in the state increases, California would face a shortage of mental health professionals between 2016 and 2028. If the total number of people entering mental health professions does not increase, these projections show that the supply of mental health professionals could fall short of demand for mental health professionals by between 12 percent and 40 percent by 2028. As we describe below, the state has recently experienced growth in the number of masters- and doctoral-level professional mental health graduates. (Professional mental health graduates generally include those intending to pursue careers in clinical care as opposed to research.)
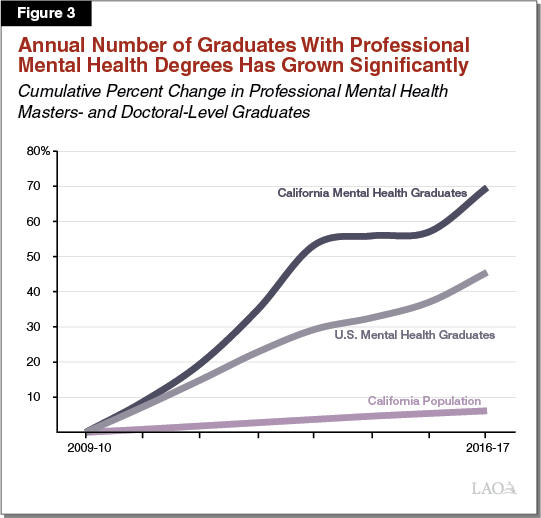
Recent Growth in Professional Mental Health Graduates Brings Uncertainty to Whether the State Is Facing a Shortage. To see whether the number of people entering mental health professions has in fact remained constant in recent years (which would suggest that the education and training of new mental health professionals is likely not meeting the state’s workforce needs), we reviewed data on the number of individuals graduating with professional masters or doctoral degrees in mental health-related fields from California universities. As shown in Figure 3, from 2009‑10 to 2016‑17, the annual number of professional degree graduates in the fields of clinical psychology, social work, counseling, and psychiatric nursing increased from 4,700 to around 8,000—a 70 percent increase. (Over this same time period, California’s resident population increased by about 6 percent.) If sustained, this increase in the number of graduates may, but is not guaranteed to, significantly ameliorate the projected mental health workforce shortage that does not necessarily assume an increase. More than 80 percent of the increase in professional mental health graduates is from graduates of private universities in the state, which do not rely on augmentations in state funding to grow enrollment.
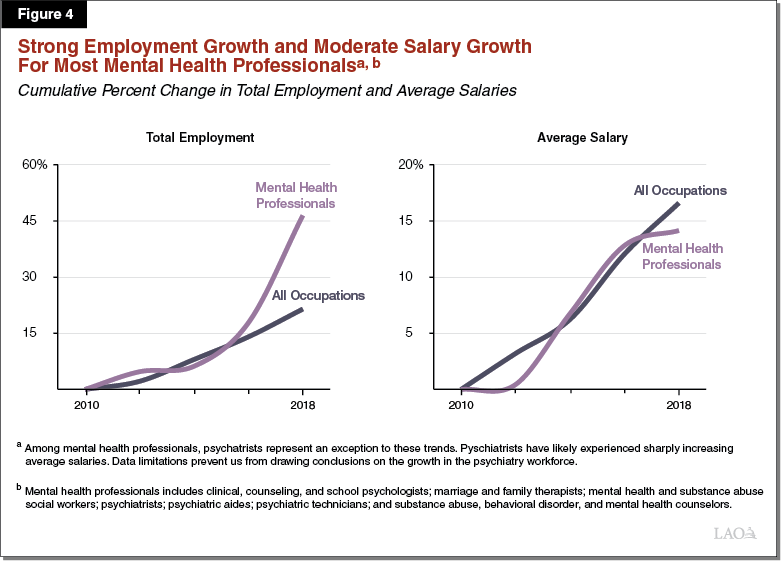
Moderate Salary Growth for Mental Health Professionals Does Not Suggest There Is a Statewide Shortage. In addition, we would expect that a shortage of mental health professionals might lead to sharply rising salaries for mental health professionals as hospitals, clinics, counties, and other organizations compete to fill needed mental health positions. We reviewed data from the Bureau of Labor Statistics, which showed that between 2010 and 2018 mental health professionals’ average salaries have increased in California at about the same rate as all occupations throughout the California economy, contrary to what we would expect under a shortage. Moreover, over this same time period, the number of mental health professionals has increased by about 50 percent. Figure 4 displays these trends for mental health professionals compared to all occupations. These trends overall do not suggest that the state is facing a statewide shortage of mental health professionals.
Stronger Evidence of Inadequate Supply of Psychiatrists Statewide. Evidence from a variety of sources suggest that California may currently or in the near future face a shortage of psychiatrists. UCSF researchers found that a significant number of psychiatrists are nearing retirement age. In addition, Bureau of Labor Statistics data do not show an increase in the number of psychiatrists in the state between 2010 and 2018. At the same time, average psychiatrists’ salaries appear to have increased to a much greater degree than all occupations throughout California, suggesting there could be significant competition for a potentially limited number of psychiatrists in the state. We would note that non-psychiatrists, such as psychologists and psychiatric technicians, can perform some of the same diagnosis-related and therapeutic tasks as psychiatrists. As such, hospitals, clinics, counties, and other organizations can utilize non-psychiatrists in place of psychiatrists. However, other than psychiatric nurse practitioners (whose statewide employment numbers and salaries we were not able to obtain data to evaluate), psychiatrists are one of the only specialized mental health professionals whose scope of practice allows them to prescribe medication. Accordingly, psychiatrists play a critical role in the mental health services delivery continuum.
Regional Disparities Exist in the Mental Health Workforce
Regional Disparities Exist Among Mental Health Professionals Overall. Although we find mixed evidence of a statewide shortage of most mental health providers, we do find strong evidence that mental health professionals are unequally distributed across the state. Figure 5 shows certain regions have a high number of overall mental health professionals per 100,000 residents relative to the state average. For example, the Greater Bay Area has almost 50 percent more mental health professionals on a population basis than the statewide average. Other regions, such as Los Angeles and the Sacramento area, have comparable numbers of mental health professionals to the statewide average. Certain regions, however, have very low numbers of mental health professionals. The Inland Empire and San Joaquin Valley regions have about two-thirds as many mental health professionals on a population basis as the statewide average, or about half as many mental health professionals on a population basis as the Greater Bay Area.
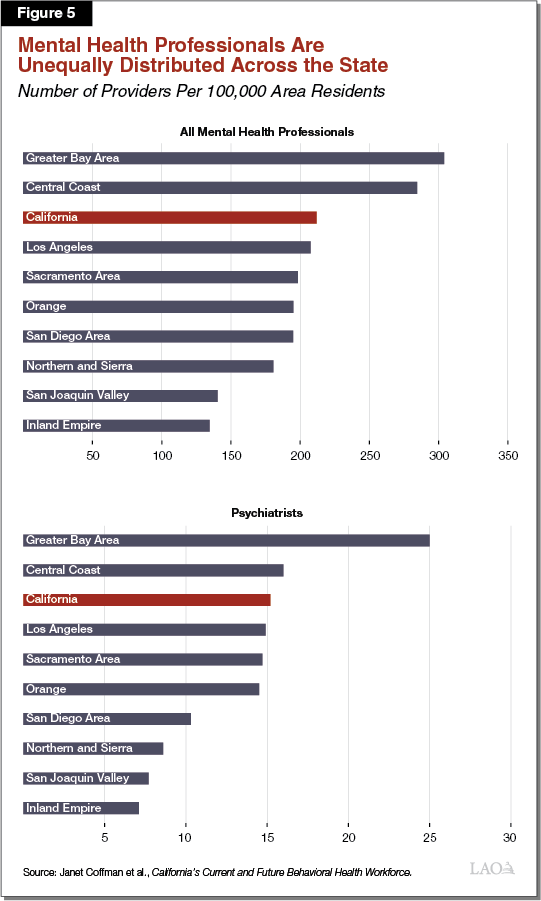
Distribution of Psychiatrists Throughout the State Is Particularly Disparate. Regional disparities of psychiatrists are greater than for mental health professionals overall. While the Greater Bay Area has 70 percent more psychiatrists than the statewide average, the Inland Empire and San Joaquin Valley have only about 50 percent of the statewide average on a population basis.
Unclear to What Extent Regional Disparities Reflect Differences in Demand for Mental Health Services. While there is strong evidence of regional disparities in terms of the supply of mental health professionals, it is unclear to what extent different regions have different demand or needs for mental health services. For example, the population of the Greater Bay Area may desire or need more mental health services than the population of San Diego. Accordingly, while the disparities in the supply of mental health professionals suggest some regions may be experiencing relatively more acute workforce shortages, additional analysis is needed to determine which regions are facing workforce challenges relative to the demand or need for mental health services.
Potential Impact of Funding Under the Governor’s Proposal Is Uncertain
Detail Lacking on How Governor’s Proposed Funding Would Be Allocated. Key details are missing on how both the $50 million in General Fund and the $100 million in MHSA funding proposed by the Governor would be allocated among existing mental health workforce programs. For example, the administration has not released a plan for how much of the MHSA funding would support state versus regional workforce programs. Of the funding for state programs, it remains unclear how much would be allocated to the various existing state programs, each of which employs different strategies and supports different sets of mental health professionals. For example, funding the Steven M. Thompson Program would fund student loan repayment exclusively for psychiatrists while funding for the WET Educational Stipend Program would support clinical rotations for a variety of professionals including social workers, psychologists, and psychiatric nurse practitioners. It is our understanding that, under the Governor’s proposal, an allocation plan for the funding would be developed in the months following the enacted budget.
Uncertainty Around Whether Existing State Programs and Strategies Have Been Effective. Overall, existing state mental health workforce programs may have had some positive impact in increasing the overall number of mental health professionals throughout the state. However, in the time available to perform this analysis, we were unable to perform a comprehensive evaluation of the impact that existing state mental health workforce programs have had on the overall supply and distribution of the state’s mental health workforce. To our knowledge, OSHPD, which oversees the mental health workforce issues and programs, has not released a comprehensive analysis of the programs’ impact (though we note that the 2020‑25 WET Five-Year Plan does include some preliminary analysis of the impact of the previous round of WET funding). For this analysis, we reviewed data on where recipients of mental health workforce stipends or student loan repayments worked after their service obligations had expired. As Figure 6 shows, this data showed little relationship between the regions of the state experiencing the greatest workforce challenges and the work locations of award recipients following the completion of their service obligations.
Figure 6
Regions With the Smallest Mental Health Workforces Have Not Seen the Largest Workforce Gains Under OSHPD’s Programs
|
Region |
Rank |
|
|
Region With the Smallest Mental Health Workforcesa |
Region With the Most Award Recipientsb |
|
|
Inland Empire |
1 |
8 |
|
San Joaquin Valley |
2 |
5 |
|
Northern and Sierra |
3 |
1 |
|
San Diego |
4 |
6 |
|
Orange |
5 |
7 |
|
Sacramento |
6 |
4 |
|
Los Angeles |
7 |
3 |
|
Central Coast |
8 |
2 |
|
Greater Bay Area |
9 |
9 |
|
aNumbers reflect the ranking of regions in terms of the size of their mental health workforces, controlling for their population sizes. A ranking of 1 applies to the region with the smallest mental health workforce and a ranking of 9 applies to the region with the largest mental health workforce. bNumbers reflect the ranking of regions in terms of where beneficiaries of OSHPD mental health workforce, education, and training programs practice following the completion of their service obligations (controlling for the regions’ population sizes). A ranking of 1 applies to the region where the most awardees practice and a ranking of 9 applies to the region where the fewest awardees practice. OSHPD = Office of Statewide Health Planning and Development. |
||
Options for the Legislature
In this section, we provide several options for legislative consideration related to the Governor’s two proposals: (1) take pause and study the underlying workforce issues further before appropriating funding, (2) scale back the requested funding level, (3) adopt the Governor’s proposals but add parameters designed to improve effectiveness, and (4) provide flexible funding to counties facing the most acute shortages. We describe these options further below. We note that the first two options would free up General Fund or MHSA funding for other priorities of the Legislature. In addition, these two options could provide a lesser amount of funding for the provision of mental health services broadly than under the Governor’s proposal.
Take Pause to Identify Workforce Needs and Cost-Effectiveness of Strategies
Identify Workforce Needs and Strategies Before Providing New State Funding. We have a number of outstanding questions related to (1) the magnitude, geography, and causes of any current or future mental health workforce shortages and (2) the effectiveness and associated trade-offs of alternative policy solutions to addressing potential mental health workforce shortages. For example, an important, open question that our analysis was unable answer is what impact psychiatric health nurses and nurse practitioners have in mitigating potential mental health workforce shortages throughout the state. Given this and other outstanding questions and uncertainties, the Legislature could reject the Governor’s proposed funding and instead direct OSHPD or another qualified entity to study the state’s mental health workforce and recommend policy solutions to ameliorate any identified issues.
In Meantime, Counties Can Use Local MHSA Funding to Meet Local Workforce Needs. To the extent that counties wish to dedicate funding to mental health workforce programs, they could use a portion of their local MHSA funding to support local mental health workforce programs. We would note that until 2018‑19, most funding for mental health workforce comprised local MHSA funding redirected by the state to mental health workforce programs.
Scale Back Funding
Counties Have Historically Shared in the Costs of Mental Health Workforce Development. Historically, a portion of what otherwise would have been local MHSA funding for counties was redirected to fund state mental health WET programs. In addition, counties are free to dedicate up to a maximum of 15 percent of MHSA funding to workforce programs. However, under the Governor’s proposal, only funding designated for state purposes (General Fund and the portion of MHSA funding dedicated to state activities and programs) would be used to support mental health workforce development. While counties have very likely already dedicated significant portions of existing MHSA funding to non-workforce programs, the most recent estimates show that MHSA revenues for counties have increased by around $600 million over the last two fiscal years combined. Given this substantial recent revenue growth, it is likely that counties have some additional revenue that remains uncommitted.
Consider, as Currently, Letting Counties Fund at Least a Portion of Their Own Local Mental Health Workforce Programs. The Legislature could consider reducing the amount of funding proposed by the Governor, while letting counties use their local MHSA funding to support local mental health workforce programs, as is currently authorized. (This option would not require any statutory changes since counties are currently authorized to spend up to around 15 percent of the funding they receive through the MHSA on mental health workforce programs.) Under this option, the Legislature could consider limiting state funding to programs and strategies that serve broader, statewide concerns, such as the training of additional mental health professionals. Here, counties could take on a greater role in funding programs that may largely serve to shift the geographic distribution of mental health professionals throughout the state, such as student loan repayment programs. Under this option, counties, would have to choose whether to dedicate their own local mental health services funding to workforce programs or to other priorities. Accordingly, it is uncertain the extent to which counties would dedicate local funding to workforce programs.
Alternatively, Consider Requiring a Local Funding Contribution. The Legislature could also consider reducing the amount of state funding provided for mental health workforce development and instead require a financial contribution from counties that ensures similar total funding as under the Governor’s proposal. Below, we summarize two approaches that the Legislature could consider.
Require a County Share of Cost. The Legislature could consider requiring counties to share in the cost of the state mental health workforce programs from which they directly benefit. For example, rather than exclusively supporting a county clinician’s student loan repayment or clinical rotation stipend with state funding, the Legislature could require counties to share in these costs. This approach would serve the overarching objective of expanding resources for mental health workforce development while also ensuring that state resources are drawn to programs and strategies that counties themselves find worthy of investment. To ensure state resources go to the areas of greatest need, different cost-sharing ratios could be applied to high-need versus low-need regions of the state. While this approach would bring benefits such as those listed above, we recognize it could bring administrative complexity.
Redirect a Portion of the Growth in MHSA Revenues to Fund Workforce Programs. In recognition that counties have likely committed much of their existing MHSA funding to various priorities, the Legislature could consider redirecting to mental health workforce programs a portion of the growth in MHSA revenue that counties would otherwise receive. This could be done retroactively for the most recent year (the period for which the funding is least likely to have been committed) or prospectively for future years. Prospectively, for example, the Legislature could consider redirecting an amount of funding that is greater than a percentage of year-over-year growth that the Legislature deems sufficient for counties to receive.
Approve Funding, but Establish Parameters for How Funding Is Allocated
Under the Governor’s proposals, the administration would have significant discretion to determine whether the funding goes to state programs or regional partnerships, as well as how it is allocated among state programs, which employ different strategies and support different professions. Provided the Legislature wishes to provide funding for mental health workforce development, the Legislature could consider what parameters it would like to set for the appropriation. The following bullets provide parameters that the Legislature might consider including in budget-related language:
Prioritize Regions With Most Acute Shortages. As previously noted, our preliminary analysis has revealed that certain regions of the state—most notably the Inland Empire and the San Joaquin Valley—are likely experiencing the most acute shortages. Nevertheless, existing mental health workforce programs at OSHPD have not necessarily proven effective in increasing the workforce in these potentially high-need regions. To ensure this funding goes to the areas with the highest need, the Legislature might consider directing OSHPD to prioritize regions with acute shortages in future funding rounds.
Target Funding Toward “Prescribing” Professions. As discussed earlier, our preliminary analysis suggests potentially greater shortages among psychiatrists compared to non-psychiatrist mental health professionals. As such, the Legislature might consider dedicating a significant portion of the funding to programs targeting the training and/or recruitment of psychiatrists. The Legislature could also consider targeting the funding toward psychiatric nurse practitioners since, given their ability to prescribe medication, they can also provide a key specialized service delivered by psychiatrists. For example, such funding could support student loan repayment programs for either or both of the two prescribing professions, residencies for psychiatrists, or clinical rotations for psychiatric nurse practitioners.
Extend Service Obligations. As previously noted, existing state mental health workforce programs generally require one-to-two year service obligations by awardees in designated shortage areas and other specified locations. Anecdotally, we have heard that awardees sometimes fulfill their service obligations and soon thereafter move to other practice locations and/or private practice to earn higher pay. To slow the rate of exit from the public mental health system as well as from high-need regions of the state, the Legislature could consider extending awardees’ service obligation requirements beyond one-to-two years.
Ensure Against Awarding Transfers From High-Need Regions. Currently, awardees may have previously worked in one county facing a mental health workforce shortage and moved to work in another—and be eligible for an award. In such a case, the award would help to change which county is facing a workforce challenge but not relieve the state’s workforce issue as a whole. The Legislature might consider restricting eligibility for awards to individuals moving from out-of-state or from regions of the state facing less severe shortages.
Provide Flexible Funding to Counties Facing Most Acute Workforce Challenges
The Legislature could consider redirecting all or a portion of the funding proposed by the Governor to instead provide flexible funding to counties facing the most acute workforce challenges, which these counties could use in accordance with local needs and conditions. For example, counties could choose to use such funding to support local education and training programs, student loan repayments, or improve pay in areas where they are facing acute recruiting challenges. To the extent that the Legislature considers the underlying problem to stem from insufficient overall funding of mental health services in certain counties, this approach would more directly address the underlying problem.
