LAO Contact
Update (2/7/22): Time requirement for incentive payment to IHSS providers in the state’s HCBS spending plan has been updated.
February 2, 2022
The 2022-23 Budget
In-Home Supportive Services
Summary. This post describes the Governor’s budget assumptions and proposals related to the In‑Home Supportive Services (IHSS) program and offers relevant issues for Legislative consideration.
Background
Overview of the IHSS Program. The IHSS program provides personal care and domestic services to low‑income individuals to help them remain safely in their own homes and communities. In order to qualify for IHSS, a recipient must be aged, blind, or disabled and in most cases have income below the level necessary to qualify for the Supplemental Security Income/State Supplementary Payment cash assistance program (for example, about $1,040 a month for an aged and/or disabled individual living independently in 2021‑22). IHSS recipients generally are eligible to receive up to 283 hours per month of assistance with tasks such as bathing, dressing, housework, and meal preparation. Social workers employed by county welfare departments conduct an in‑home assessment of an individual’s needs in order to determine the amount and type of service hours to be provided. In most cases, the recipient is responsible for hiring and supervising a paid IHSS provider—oftentimes a family member or relative. The average number of service hours that will be provided to an estimated 598,000 IHSS recipients is projected to be 120 hours per month in 2022‑23.
IHSS Costs Split Between Federal Government, State, and County. IHSS costs are shared by the federal government, state, and county. Since IHSS primarily is delivered as a Medi‑Cal benefit, the federal share of cost is determined by the Medicaid reimbursement rate, which typically is 50 percent. The state receives an enhanced federal reimbursement rate for many IHSS recipients who receive services as a result of the Patient Protection and Affordable Care Act expansion (90 percent federal reimbursement rate) and the Community First Choice Option waiver (56 percent federal reimbursement rate). Overall, the effective federal reimbursement rate for IHSS is about 54 percent. The remaining nonfederal share of IHSS costs is covered by the state and counties. Historically, counties paid 35 percent of the nonfederal share of IHSS service costs and 30 percent of the nonfederal share of IHSS administrative costs. Beginning in 2012‑13, however, the historical county share‑of‑cost model was replaced with an IHSS county maintenance‑of‑effort (MOE), meaning county costs would reflect a set amount of nonfederal IHSS costs as opposed to a certain percent of nonfederal IHSS costs. The state is responsible for covering the remaining nonfederal share of costs not covered by the IHSS county MOE.
Budget Overview and LAO Assessment
The Governor’s budget proposes a total of $18.5 billion (all funds) for IHSS in 2022‑23, which is about $1.6 billion (9 percent) above estimated expenditures in 2021‑22. The budget includes about $6.5 billion from the General Fund for support of the IHSS program in 2022‑23. We estimate that this is a net increase of about $2.8 billion (75 percent) above estimated General Fund costs in 2021‑22. This year‑to‑year increase in General Fund reflects a much faster rate of cost growth relative to prior budget estimates. The main reason for the year‑to‑year General Fund cost increase is the anticipated ramp down of temporary increases to federal Medicaid funds (largely associated with the public health emergency) that were used to offset General Fund costs in the IHSS program in 2021‑22. This ramp down results in roughly $2 billion in IHSS costs shifting back to the General Fund in 2022‑23. Additionally, the Governor’s budget assumes continued year‑to‑year growth in the three primary IHSS cost drivers: caseload (2.8 percent), hours per case (1 percent), and IHSS provider hourly wages and benefits (3 percent). We describe in more detail key cost increases and cost shifts in this section.
IHSS Paid Caseload, Hours Per Case, and Hourly Wage Assumptions
LAO Bottom Line: Growth in IHSS Caseload Continues to Be Slower Than Pre‑COVID‑19 Rates. Caseload growth, a rising number of paid hours per case, and hourly wage increases for IHSS providers are key drivers of increasing IHSS costs. Based on our analysis, we found that hourly wages and hours per case generally continue to grow at a rate similar to historical levels. However, we found that IHSS paid caseload continues to grow at a slower rate relative to pre‑COVID‑19 growth trends. Below, we summarize our assessment of the paid caseload, hours per case, and hourly wage assumptions included in the Governor’s budget.
Changes in Caseload Trends Before and After the Onset of the Pandemic. Figure 1 summarizes our analysis of IHSS caseload trends before and after the onset of the pandemic. In general, the current average number of new applicants and denials are similar to pre‑COVID‑19 levels. In contrast, the average number of terminations are below pre‑COVID‑19 levels, which in part is due to the temporary pause of Medi‑Cal redeterminations (which we discuss in more detail in a later section). Additionally, authorized cases continue to grow at a similar rate to pre‑COVID‑19 levels (4 percent annually, or roughly 25,000 more authorized cases every year). We found, however, that IHSS paid caseload is growing at a slower rate since the start of COVID‑19 (from 4 percent annually to 2 percent in 2020‑21).
Figure 1
Assessment of IHSS Caseload Trends
|
IHSS Caseload Trend |
IHSS Caseload Trends… |
Comparison |
|
|
...Before COVID‑19 |
...Since COVID‑19 |
||
|
Average number of new IHSS applications |
Around 17,000 in any given month. |
Around 17,000 in any given month. |
Generally reflects pre‑COVID‑19 trends. |
|
Average number of IHSS denials |
Around 7,500 in any given month. |
Around 7,500 in any given month. |
Generally reflects pre‑COVID‑19 trends. |
|
Average number of IHSS terminations |
Around 9,000 in any given month. |
Around 5,000 in any given month. |
Falls below pre‑COVID‑19 trends. |
|
Average growth in authorized cases |
About 4 percent annually. |
About 4 percent in 2020‑21. |
Generally reflects pre‑COVID‑19 trends. |
|
Average growth in paid cases |
About 4 percent annually. |
About 2 percent in 2020‑21. |
Falls below pre‑COVID‑19 trends. |
|
IHSS = In‑Home Support Services. |
|||
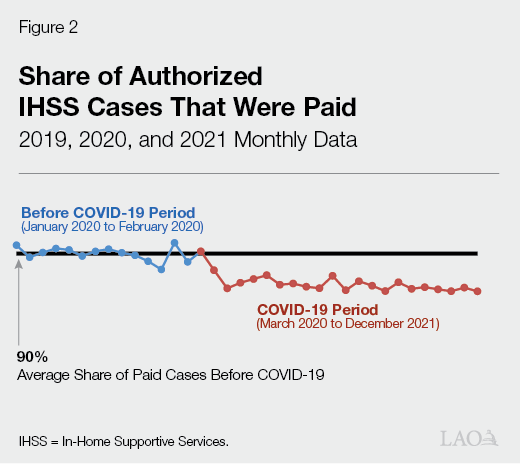
Continued IHSS Paid Caseload Growth, but at a Slower Rate. Prior to the start of COVID‑19, the average number of IHSS paid cases has grown at an average rate of about 4 percent annually, reaching 555,000 in 2019‑20. The Governor’s budget, however, assumes slower paid caseload growth in 2021‑22 (2.8 percent) and 2022‑23 (2.7 percent). IHSS paid caseload began to grow at a slower rate in 2020‑21 (2.1 percent), which coincided with the start of the COVID‑19 pandemic (March 2020). Based on our analysis of caseload data, the slower growth in IHSS paid cases seems to be due, in part, to fewer authorized cases receiving paid services in any given month since the start of COVID‑19. Figure 2 shows that the average share of authorized cases that are paid every month slightly decreased from 90 percent to 88 percent since March 2020. This translates to roughly 14,000 fewer paid cases every month relative to pre‑COVID‑19 levels. Some of the reasons why authorized cases may not receive paid services include recipients not yet hiring an IHSS provider or being temporarily hospitalized or admitted into a licensed care facility. Additionally, one possible COVID‑19‑related reason may be that recipients with non‑live‑in providers or non‑live‑in providers themselves may be hesitant to interact with individuals outside of their household due to public health concerns. We are working with Department of Social Services (DSS) to get additional IHSS caseload data and will provide further comments at the time of the May Revision.
Continued Growth in IHSS Hours Per Case. Since 2016‑17, the number of IHSS paid hours per case increased by about 2.5 percent annually, reaching 118.7 hours per case in 2020‑21. The Governor’s budget estimates that average hours per case will remain roughly the same in 2021‑22 and slightly increase in 2022‑23 by 1 percent (to 119.6 hours per case). Based on recent growth trends, we expect that the average paid hours per case will continue to grow in 2021‑22 (as opposed to remaining roughly flat). Additionally, we expect the growth in average hours per case in 2022‑23 to be slightly higher than the administration’s current estimate. We will continue to monitor the data related to IHSS paid hours per case and provide further comments at the time of the May Revision if necessary.
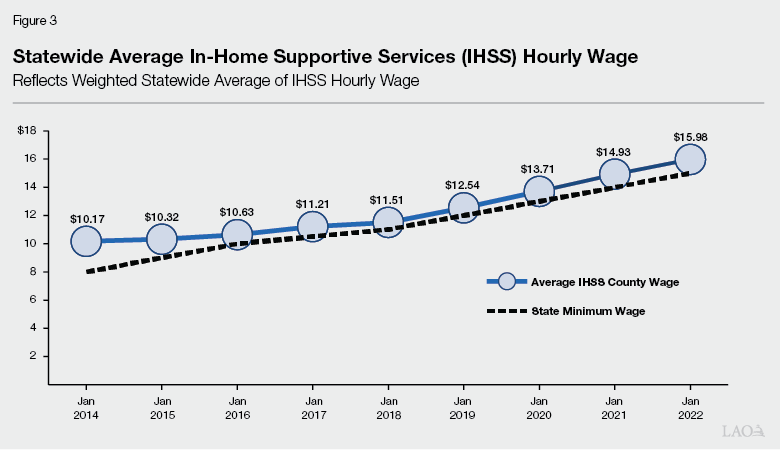
Continued Growth in IHSS Wages. As shown in Figure 3, the average IHSS hourly wage has increased by 6 percent annually since 2014. The growth in IHSS hourly wages in part is due to increases to the state minimum wage—from $8 per hour in January 1, 2014 to $15 per hour in January 1, 2022. Pursuant to current law, the state minimum wage will remain at $15 per hour in January 1, 2023, increasing by inflation annually beginning January 1, 2024. Additionally, counties may establish IHSS hourly wages above the state minimum wage through local wage ordinances or, more commonly, collectively bargained agreements. As of January 2022, 50 counties have IHSS hourly wages above the state minimum wage ($15 per hour). The Governor’s budget includes about $400 million General Fund ($877 million total funds) in 2022‑23 for IHSS previously set, or agreed upon, wage increases. Specifically, this cost estimate partially reflects the full‑year impact of the state minimum wage increase to $15 per hour (effective January 1, 2022). Additionally, the Governor’s budget includes the full‑year cost impact of locally negotiated wage increases above the $15 per hour state minimum wage.
Temporary Pause of Medi‑Cal Redeterminations
LAO Bottom Line: Consider Ways to Address Different Treatment for IHSS Recipients Who Fail to Complete Medi‑Cal Redetermination Once Federal Pause Expires. Medi‑Cal redeterminations were paused during the COVID‑19 public health emergency. Once Medi‑Cal redeterminations begin again, some IHSS recipients who do not complete their Medi‑Cal redetermination may move to the IHSS‑Residual program (fully state‑funded IHSS program), while others may lose their eligibility for IHSS. The Legislature could consider ways to ensure all recipients receive the same treatment, which we explain in more detail below.
Anticipated Expiration of Temporary Pause of Medi‑Cal Redeterminations and Subsequent IHSS Terminations. Federal COVID‑19‑related legislation effectively requires the state to suspend most Medi‑Cal eligibility redeterminations for the duration of the national public health emergency declaration, which the Governor’s budget assumes will last until June 30, 2022. While Medi‑Cal redeterminations are paused, essentially no IHSS recipient would need to be eliminated from IHSS due to failure to complete their Medi‑Cal redetermination. This effectively reduced the number of terminated IHSS recipients and the number of IHSS recipients entering the IHSS‑Residual program. As a result, the Governor’s budget assumes $90 million General Fund savings for the IHSS‑Residual program in 2021‑22.
Consider Possible Ways to Ensure Similar Treatment When Pause on Medi‑Cal Redeterminations Expires. When IHSS recipients do not complete the Medi‑Cal redetermination process they can continue to receive their IHSS services through the IHSS‑Residual program unless counties manually terminate them from the IHSS program. Those that are terminated from the program must reinstate their Medi‑Cal eligibility before receiving services again. Currently, there is no consistent approach to manual terminations. As a result, some recipients continue to receive services through the IHSS‑Residual program, while others do not.
When the pause on Medi‑Cal redeterminations expires, there likely will be an increase in Medi‑Cal terminations due to beneficiaries not completing the redetermination process. We expect that in some cases, IHSS recipients terminated from Medi‑Cal will continue to receive services through the residual program, while others will not. As a part of the 2021‑22 budget, the Legislature did not approve the administration’s approach to address this different treatment (which was to automatically terminate all IHSS recipients who do not complete their Medi‑Cal redetermination and require them to reinstate their Medi‑Cal eligibility before reentering the IHSS program). Given the continued possibility of differing treatment across similar recipients, the Legislature may want to consider the benefits and trade‑offs of alternative approaches to ensure similar treatment for all recipients. For example, the Legislature could consider ways to assist IHSS recipients in completing their Medi‑Cal redetermination or provide temporary IHSS services for all IHSS recipients while they work towards reestablishing their Medi‑Cal eligibility.
Temporary Increase to Federal Medicaid Funding
LAO Bottom Line: IHSS General Fund Costs Expected to Increase in 2023‑24 as a Result of Expiration of Temporary Increase in Federal Medicaid Funding. Under the Families First Coronavirus Response Act, the federal government increased the federal match rate for Medicaid services by 6.2 percentage points for the duration of the national public health emergency caused by COVID‑19. This increased federal match lowers state costs for Medi‑Cal, IHSS, and other programs that rely on federal Medicaid funding. The Governor’s budget assumes this enhanced federal funding is in place from January 1, 2020 through June 30, 2022 and will offset $940 million in total IHSS General Fund spending in 2021‑22.
Additionally, under the American Rescue Plan (ARP) Act, the federal government increased the federal match rate for IHSS and other Medicaid‑funded home‑ and community‑based services (HCBS) by an additional 10 percentage points from April 1, 2021 through March 31, 2022. This increase in federal Medicaid funding is expected to offset over $1 billion in baseline IHSS General Fund spending across 2020‑21 and 2021‑22. These savings will be transferred to the HCBS ARP Fund and spent on federally approved HCBS enhancements and expansions. The Governor’s budget reflects the baseline IHSS savings and transfer of funds in the Department of Health Care Services budget.
Status of COVID‑19 Program Responses and Flexibilities
LAO Bottom Line: Consider Whether Certain COVID‑19 Program Flexibilities Merit an Extension. The state implemented numerous IHSS program flexibilities and enhancements to mitigate health and safety risks associated with COVID‑19. As shown in Figure 4, many of these program flexibilities and enhancements have expired. Given that Omicron has become the prevailing COVID‑19 variant in California since the development of the Governor’s budget, the Legislature may want to consider whether any IHSS program flexibilities or temporary supports warrant an extension.
Figure 4
Status of COVID‑19 IHSS Program Responses and Flexibilities
|
Program Activity |
Description of Flexibility |
End Date |
|
Active |
||
|
Initial IHSS Assessment |
Counties may use video‑conferencing for initial assessment only if an applicant or someone in the applicant’s household has been infected with COVID‑19, has symptoms of COVID‑19, or has been exposed to COVID‑19 in the previous two weeks. In situations where there is less risk of COVID‑19 infection, counties should conduct initial assessment via an in‑person home visit. Counties may collect as much information as possible regarding the applicant over the phone before the home visit to reduce the amount of time spent in the applicant’s home. |
End of the state of emergency in California |
|
Annual IHSS Reassessment |
While counties are expected to begin to transition back to in‑person reassessments whenever possible, they may continue to use telephone and video‑conferencing to conduct annual reassessments as needed. Additionally, before conducting an in‑person reassessment, counties may collect as much information as possible regarding the applicant over the phone to reduce the amount of time spent in the applicant’s home. |
End of the state of emergency in California |
|
Submission of IHSS Program Forms |
When assessments and reassessments are conducted via telephone or video‑conference, county staff may accept self‑attestations from applicants and recipients and/or their authorized representatives in lieu of original signatures on most required forms normally signed during assessments and reassessments. |
End of the state of emergency in California |
|
Submission of IHSS Provider Identification Documents |
Temporarily waive requirement for IHSS providers to go to IHSS county or public authority office to present and photocopy original identification documents if office is closed. As an alternative, counties may accept mailed‑in or faxed photocopies of the original identification documentation. |
End of the state of emergency in California |
|
Quality Assurance and Program Integrity |
Counties may perform home visits for purposes of quality assurance and program integrity remotely using telehealth, including video‑conferencing and telephone. Specifically, counties should continue to use video‑conferencing in situations where the applicant or someone in their household has been infected with COVID‑19, has symptoms of COVID‑19, or has been exposed to COVID‑19 in the two weeks prior to the home visit. In situations where there is no danger of COVID‑19 infection, the county can conduct an in‑person home visit. |
End of the state of emergency in California |
|
Expired |
||
|
Implement Adverse Actions Related to IHSS Reassessments |
Postpone the implementation of adverse actions, such as reduction of IHSS hours and termination from IHSS program, resulting from the IHSS redetermination. |
June 30, 2020 |
|
Social Worker Outreach |
IHSS and APS social workers perform out‑bound calls and/or visits to elderly recipients to ensure at‑risk recipients are receiving services they need and are safe in their homes. |
June 30, 2020 |
|
IHSS Provider Criminal Background Check |
Temporarily suspend requirement for IHSS provider to complete fingerprint‑based criminal background check. As an alternative, counties may conduct name‑based criminal background checks. |
July 31, 2020 |
|
IHSS Paid Parent Provider Eligibility |
Allow IHSS parent provider in two‑parent household to continue to be an eligible IHSS provider even if the second parent becomes a suitable care provider because the parent is not working or attending school or vocational program. |
August 3, 2020 |
|
In‑Person Provider Orientation |
Temporarily suspend requirement for IHSS providers to complete in‑person provider orientation. |
August 31, 2020 |
|
IHSS Provider Overtime Violations |
Temporarily remove violations if IHSS provider worked above the allowable overtime limit. |
August 31, 2020 |
|
Federal COVID‑19 Paid Sick Leave |
Provide additional hours of paid sick leave for IHSS providers if they are unable to work due to COVID‑19. |
March 31, 2021 |
|
Back‑Up Provider System |
Create a statewide emergency back‑up provider system with $2 per hour wage differential. |
December 31, 2021 |
|
COVID‑19 Vaccination Assistance |
Pay IHSS provider to accompany IHSS recipient to their COVID‑19 vaccination appointment. |
December 31, 2021 |
|
Note: There is no set end date for the state of emergency in California. IHSS = In‑Home Supportive Services and APS = Adult Protective Services. |
||
Permanent Back‑Up Provider System
LAO Bottom Line: Consider Possible Ways to Address Gap in IHSS Back‑Up Provider Services Given Delay in Permanent Back‑Up Provider System. The emergency back‑up provider system expired on December 31, 2021. While the permanent back‑up provider system was intended to take effect on January 1, 2022, because no program structure has been set in statute yet, the start date has been delayed to July 1, 2022. As a result, there is a current gap in back‑up provider services. Below, we describe possible ways the Legislature could address this gap in back‑up provider services.
Lacking Statutory Structure, Permanent Back‑Up System Delayed. At the start of the COVID‑19 pandemic, the state created a temporary back‑up provider system to assist IHSS recipients when their regular provider could not work due to circumstances related to COVID‑19. The temporary COVID‑19 back‑up provider system expired on December 31, 2021. The 2021‑22 budget included $5 million General Fund to create a permanent back‑up provider system on January 1, 2022, contingent on a policy framework being adopted in statute. However, a policy framework for the permanent back‑up provider system has not yet been adopted, resulting in a lapse in statewide back‑up provider services. (Some counties are continuing to provide back‑up provider services despite the expiration of the temporary COVID‑19 back‑up provider system.) We understand that the administration intends to propose trailer bill language—effective July 1, 2022—outlining the program structure for the permanent back‑up provider system. The Governor’s budget includes $11 million General Fund in 2022‑23 to implement the permanent back‑up provider system on July 1, 2022.
Possible Ways to Address Gap in IHSS Back‑Up Provider Services. In the meantime, the Legislature could consider ways to address the current gap in statewide back‑up provider services. For example, the Legislature could extend the expenditure authority of any unspent funds originally provided for the temporary emergency back‑up provider system to June 30, 2022. (Recently, the administration extended the expenditure authority for existing essential protective gear funds from December 31, 2021 to June 30, 2022 via an all‑county letter. A similar approach could possibly be used to extend the expenditure authority of any unspent back‑up provider service funds.) Alternatively, the Legislature could allow the $5 million General Fund allocated in the 2021‑22 budget to be used for emergency back‑up provider services until a permanent system is established or adopt the administration’s permanent back‑up provider system proposal early (to the extent that the proposed language reflects Legislative goals).
Proposed Full‑Scope Medi‑Cal Expansion to
Remaining Undocumented Adults
LAO Bottom Line: Proposed Full‑Scope Medi‑Cal Expansion to Remaining Undocumented Adults Would Increase IHSS Caseload. Historically, income‑eligible undocumented immigrants only qualified for “restricted‑scope” Medi‑Cal coverage, which covers their emergency‑ and pregnancy‑related service costs. In general, beneficiaries of restricted scope Medi‑Cal are not eligible for IHSS. The state has expanded comprehensive, or “full‑scope,” Medi‑Cal coverage, including IHSS eligibility, to income‑eligible undocumented children (effective May 2016), adults aged 19 through 25 (effective January 1, 2020), and older adults aged 50 and over (effective no sooner than May 2022).
The Governor’s budget proposes to further extend full‑scope Medi‑Cal coverage and IHSS eligibility to income‑eligible undocumented immigrants aged 26 to 49 no sooner than January 2024. As a result of this proposal, all undocumented immigrants, regardless of age, will be eligible for full‑scope Medi‑Cal and IHSS. While no funding is provided within the budget window (2021‑22 and 2022‑23) due to the proposed schedule of implementation, the administration estimates that this policy change will increase IHSS costs over time, reaching ongoing costs of roughly $400 million General Fund in 2026‑27. (Upcoming publications, The 2022‑23 Budget: Analysis of the Medi‑Cal Budget and The 2022‑23 Budget: Analysis of Health Care Access and Affordability Proposals, will provide additional details on the full‑scope Medi‑Cal expansion to remaining undocumented adults.)
Implementation of Phasing in the Medi‑Cal Asset Limit Repeal
LAO Bottom Line: Phasing in Medi‑Cal Asset Limit Repeal Will Increase IHSS Caseload. Currently, seniors and persons with disabilities must have assets at or below $2,000 (or $3,000 for couples) to be eligible for Medi‑Cal. The 2021‑22 budget included legislation to raises the Medi‑Cal asset limit from $2,000 to $130,000 for individuals and from $3,000 to $195,000 for couples no sooner than July 2022. Moreover, the asset limit would be eliminated altogether no sooner than January 2024 if the necessary federal approvals are obtained. The Governor’s budget assumes that the asset limit will be raised on July 1, 2022, resulting in more seniors and persons with disabilities becoming eligible for Medi‑Cal services, including IHSS. The administration estimates that about 6,000 seniors and persons with disabilities will become eligible for IHSS as a result of this policy change, increasing General Fund costs by $67 million in 2022‑23.
IHSS‑Related HCBS Spending Plan Items
LAO Bottom Line: DSS Working Towards Implementation of IHSS‑Related HCBS Spending Plan Items. As previously mentioned, the ARP Act temporarily increases the federal Medicaid match for HCBS services, including IHSS. The state expects to receive, in total, $3 billion in additional federal Medicaid funds (including the estimated $1 billion in additional federal Medicaid funds for the IHSS program). As a condition of receiving these funds, the state is required to spend an equal amount of funding on new HCBS enhancements and expansions. The federal government conditionally approved the various HCBS enhancements and expansions included in the state’s HCBS spending plan. The state’s HCBS spending plan includes two IHSS‑related enhancements: (1) provide a one‑time $500 incentive payment to IHSS providers who worked at least two months between March 2020 and March 2021 and (2) create specialized training opportunities for IHSS providers. We understand that the one‑time $500 payments to IHSS providers tentatively are scheduled to occur in early 2022. Additionally, DSS is currently seeking stakeholder input on the structure of the IHSS provider training opportunities, which is set to start no later than September 1, 2022 (and remain operative until March 1, 2024).
