February 25, 2025
The 2025-26 Budget
California Department of Corrections and Rehabilitation
- Overview
- State Prison and Parole Population and Other Biannual Adjustments
- San Quentin Rehabilitation Center and The California Model
- Inpatient Mental Health Beds
- Suicide Watch
- Parole Community Rehabilitation Programs
- Air Cooling Pilot Program
- Appendix
Summary
In this brief, we assess and make recommendations on several California Department of Corrections and Rehabilitation (CDCR) budget proposals. Below, we provide a summary of our major recommendations. (A figure summarizing all of our recommendations is in the appendix of this brief.)
State Prison and Parole Population and Other Biannual Adjustments. The Governor’s budget estimates that Proposition 36 (2024), which increased punishment for various theft and drug crimes, will cause the average daily prison population to be about 570 higher (or 1 percent) than otherwise in 2024‑25 and 3,300 higher (or 4 percent) in 2025‑26. It estimates that Proposition 36 will not impact the average daily parole population in 2024‑25 but will cause the population to be about 360 higher (or 1 percent) than otherwise in 2025‑26. We identify flaws in the administration’s methodology that mean CDCR may be overbudgeted by millions of dollars in 2024‑25 and tens of millions of dollars in 2025‑26. Accordingly, we recommend directing the administration to address these flaws at the May Revision.
San Quentin Rehabilitation Center (SQRC) and the California Model. The Governor proposes a total of $7.8 million General Fund in 2025‑26 (growing to $13 million by 2027‑28) for SQRC to activate a new learning center and make various other programmatic enhancements. The proposal is part of a systemwide effort to develop the “California Model,” which is intended to reduce recidivism and improve the health and wellness of people who live and work in prison. While it is reasonable to activate the new learning center, we recommend rejecting most of the remainder of the request unless the administration is able to provide a clear plan for SQRC. In addition, we recommend requiring the administration to produce a report that answers key questions about the California Model.
Inpatient Mental Health Beds. The Governor proposes $3 million General Fund in 2025‑26 (growing to $4.4 million in 2026‑27 and ongoing) to activate a newly constructed licensed 50‑bed mental health crisis facility. With the addition of this capacity, the budget reflects operation of 686 inpatient beds in excess of the amount projected to be necessary. We recommend approving the activation to address regional bed needs, but directing CDCR to seek approval from the Coleman federal court to align statewide inpatient bed capacity with updated population projections and to account for transportation savings. These changes could save more than $100 million annually if all the excess beds are deactivated.
Parole Community Rehabilitation Programs. The Governor proposes $44.9 million General Fund in 2025‑26 (generally increasing annually thereafter) for various parole rehabilitation programs. This would support: (1) a roughly 30 percent one‑time cost‑of‑living increase for specific programs; (2) an ongoing 2 percent annual cost‑of‑living increase for those same programs; and (3) a two‑year extension of a housing program. While providing cost‑of‑living increases is reasonable, we think the Legislature could make additional changes that generate state savings from leveraging federal funds through Medi‑Cal. Accordingly, we recommend approving the proposed funding on a limited‑term basis and requiring CDCR to take steps to increase utilization of Medi‑Cal for some of these programs, which could improve them while reducing state costs. Additionally, we recommend evaluating all of these programs to determine whether they merit continued support or need to be restructured to be effective.
Overview
Roles and Responsibilities. CDCR is responsible for the incarceration of certain adults convicted of felonies, including the provision of rehabilitation programs, vocational training, education, and health care services. As of January 29, 2025, CDCR was responsible for incarcerating about 91,000 people. Most of these people are housed in the state’s 31 prisons and 34 conservation camps. The department also supervises and treats about 34,700 adults on parole and is responsible for the apprehension of those who commit parole violations. In addition, the department operates the Pine Grove Youth Conservation Camp to provide wildland firefighting skills to justice‑involved youth from counties that have entered into contracts with CDCR.
Operational Spending Proposed for 2025‑26. The Governor’s January budget proposes a total of about $13.9 billion to operate CDCR in 2025‑26, mostly from the General Fund. Figure 1 shows the total operating expenditures estimated in the Governor’s budget for the prior and current years and proposed for the budget year. As the figure indicates, the proposed spending level reflects a decrease of $149 million (1 percent) from the revised 2024‑25 level. This decrease primarily reflects expiration of previously authorized limited‑term spending. These decreases are partially offset by various proposed augmentations, such as funding to address increased costs resulting from inflation and population caseload adjustments. The proposed $149 million decrease does not reflect anticipated reductions associated with Control Sections 4.05 and 4.12 of the 2024‑25 Budget Act or increases in employee compensation costs in 2025‑26 because they are accounted for elsewhere in the budget. For more information about the reductions associated with Control Sections 4.05 and 4.12, please see our publication, The 2025‑26 Budget: State Departments’ Operational Efficiencies (Control Sections 4.05 and 4.12). The proposed budget would provide CDCR with a total of about 60,000 positions in 2025‑26, a decrease of about 475 (less than 1 percent) from the revised 2024‑25 level.
Figure 1
Total Expenditures for Operation of CDCR
(Dollars in Millions)
|
2023‑24 |
2024‑25 |
2025‑26 |
Change From 2024‑25 |
||
|
Amount |
Percent |
||||
|
Adult Institutions |
$12,809 |
$12,450 |
$12,236 |
‑$214 |
‑2% |
|
Adult Parole |
702 |
694 |
728 |
34 |
5 |
|
Administration |
914 |
787 |
818 |
31 |
4 |
|
Board of Parole Hearings |
75 |
73 |
74 |
1 |
1 |
|
Totals |
$14,499 |
$14,005 |
$13,856 |
‑$149 |
‑1% |
|
aDoes not reflect anticipated reductions associated with Control Sections 4.05 and 4.12 of the 2024‑25 Budget Act or increases in employee compensation costs in 2025‑26 because they are accounted for elsewhere in the budget. |
|||||
|
CDCR = California Department of Corrections and Rehabilitation. |
|||||
Capital Outlay Spending Proposed for 2025‑26. The Governor’s budget proposes total expenditures of $14.1 million General Fund for capital outlay projects in 2025‑26. This amount includes (1) $11.5 million to construct new groundwater wells to supply Ironwood State Prison in Blythe, (2) $1.2 million for the preliminary plans phase of a project to construct new ground water wells to supply Central California Women’s Facility and Valley State Prison in Chowchilla, and (3) $982,000 for the working drawing phase of a project to construct a potable water treatment system at the California Health Care Facility in Stockton.
State Prison and Parole Population and Other Biannual Adjustments
Background
Adjustments Proposed Biannually Based on Projected Population Changes and Other Factors. As part of the Governor’s January budget proposal each year, the administration requests adjustments to CDCR’s budget based on projected changes in the prison and parole populations in the current and budget years. The adjustments are made both on the overall population and various subpopulations (such as people housed in reentry facilities and sex offenders on parole). In addition, some adjustments include factors other than population trends, such as inflation adjustments. The administration then modifies both types of adjustments based on updated information each spring as part of the May Revision.
Governor’s Proposal
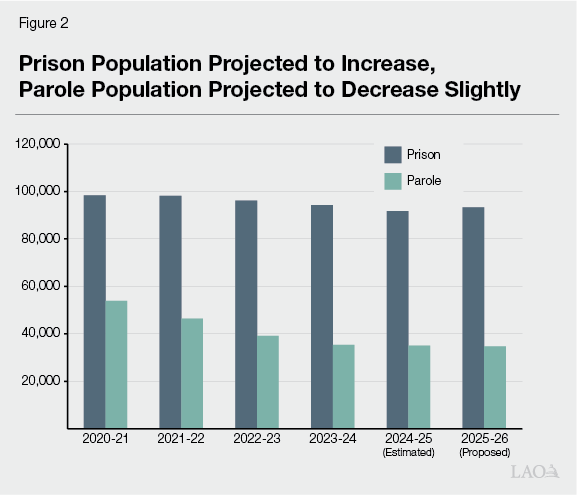
Prison Population Projected to Increase, Parole Population Projected to Decrease Slightly in 2025‑26. As shown in Figure 2, the average daily prison population is projected to be 93,300 in 2025‑26, an increase of about 1,600 people (2 percent) from the estimated current‑year level. The average daily parole population is projected to be 34,700 in 2025‑26, a slight decrease of 270 people (less than 1 percent) from the estimated current‑year level. The projected increase in the prison population is primarily due to the estimated impact of Proposition 36, which increased punishment for certain drug and theft crimes and created a new court process called a “treatment‑mandated felony” for certain people who possess illegal drugs. Specifically, the administration estimates that Proposition 36 will cause the average daily prison population to be about 570 higher (or 1 percent) than otherwise in 2024‑25 and 3,300 higher (or 4 percent) in 2025‑26. The administration estimates that Proposition 36 will have no impact on the average daily parole population in 2024‑25 but will cause it to be about 360 higher (or 1 percent) than it otherwise would be in 2025‑26.
Net Increase in Current‑Year Funding Adjustments. The Governor’s budget reflects adjustments to 2024‑25 spending, largely from the General Fund, that result in a net increase of $51 million. The current‑year net increase in costs is primarily due to both a higher total prison population and an increase in the portion of the population with high health care needs relative to what was assumed in the 2024‑25 Budget Act. This increase in costs is partially offset by various factors, including lower‑than‑expected costs of providing naloxone (a medication that can prevent overdose deaths) to people when they are released from prison and free phone calls to people in prison.
Net Increase in Budget‑Year Funding Adjustments. The budget proposes a net increase of $81 million in adjustments in 2025‑26. Similar to the current‑year, this net increase is primarily due to both a higher total prison population and an increase in the portion of the population with high health care needs relative to what was assumed in the 2024‑25 Budget Act. This increase in costs is partially offset by various factors, such as a projected decrease in costs related to the decline in the parole population.
Assessment
Impact of Proposition 36 on Prison Population Is Likely Overestimated for Current and Budget Years. The department did not provide detailed backup showing its methodology to estimate the impact of Proposition 36 on the prison population. However, based on discussions with the department, it is our understanding that CDCR used the number of people that were admitted to prison for drug possession and certain lower‑level theft crimes in 2013‑14, the year before Proposition 47 (2014) reduced prison admissions for these crimes by converting them to misdemeanors. The department then assumed that the same number of people would again be admitted to state prison under Proposition 36 and would remain in state prison for 11 months on average. We find that this estimation methodology is problematic for the following reasons:
- Does Not Account for Key Features of Treatment‑Mandated Felony. CDCR’s estimate assumes that the same number of people who were committed to prison for drug possession prior to Proposition 47 would again be committed to prison under Proposition 36. However, this is not plausible for two primary reasons. First, Proposition 36 only allows people who possess certain drugs to be charged with a treatment‑mandated felony if they have at least two past drug convictions, whereas, people who possessed drugs prior to Proposition 47 could be charged with a felony even without any prior convictions. Second, it requires that people are generally given the option of treatment in lieu of incarceration in county jail or state prison. Accordingly, the number of people that reach prison under Proposition 36 for drug possession is likely to be substantially smaller than the number of people that were sentenced to prison for drug possession prior to the passage of Proposition 47.
- Includes Crimes That Were Not Affected by Proposition 36. The methodology counts 2013‑14 prison admissions for people who were convicted of receiving stolen property. However, this crime was generally not affected by Proposition 36. Similarly, the estimate appears to include all admissions for the lower‑level theft crimes affected by Proposition 47. However, Proposition 36 only affects a subset of those cases, such as by allowing multiple acts of misdemeanor theft to be prosecuted as a felony if the combined dollar amount exceeds $950.
- Excludes Crimes That Were Affected by Proposition 36. The methodology does not include several crimes that were affected by Proposition 36. These include cases in which people receive time added to their sentence for selling high volumes of illegal drugs, being armed with a firearm during the commission of a drug felony, or selling drugs to a person who suffers significant physical injury as a result of using the drug.
The first two flaws discussed above cause the department’s methodology to overestimate the impact of Proposition 36. The third flaw causes the methodology to underestimate the impact. On net, we find that the methodology likely overestimates the impact of Proposition 36 in the current and budget years. This is because the third flaw largely involves crimes that drive a relatively smaller number of prison admissions per year but have longer lengths of stay in prison. Accordingly, the effect of the third flaw—which leads to underestimation—is likely relatively negligible for near‑term projections. Our estimates suggest that the average daily prison population impact of Proposition 36 could be in the low hundreds in 2024‑25 and grow to around 1,000 or so in 2025‑26—less than half of the magnitude of the administration’s estimates. This would cause CDCR to be overbudgeted in the millions of dollars in 2024‑25 and tens of millions of dollars in 2025‑26. However, any estimate at this early point in the implementation of Proposition 36 is subject to significant uncertainty.
Administration’s Assumption That Proposition 36 Will Impact the Parole Population in the Budget Year Is Not Plausible. People whose current offense is classified as serious or violent, as well as certain others, such as high‑risk sex offenders, are placed on state parole supervision after they are released from prison. All other people released are placed under the supervision of a county probation officer. Only two components of Proposition 36 relate to serious or violent crimes, meaning only these provisions could impact the parole population. First, Proposition 36 specified that selling drugs to a person who suffers a significant physical injury as a result of using the drug is a serious and violent crime. Second, the measure requires courts to warn people convicted of selling certain drugs that they could be charged with murder if they sell or provide illegal drugs that kill someone. This could make it more likely for them to be convicted of murder—also a serious and violent crime—in the future if they later sell drugs to someone who dies. Both of these crimes would carry relatively long prison sentences. Accordingly, it is not plausible that someone could commit one of these crimes, serve a sentence, and be released to parole before the end of 2025‑26. This means that the proposed 2025‑26 budget includes roughly a few million dollars in excess funding for parole.
Recommendation
Direct CDCR to Address Key Flaws in Its Proposition 36 Population Impact Estimates at the May Revision. We recommend that the Legislature direct the department in spring budget hearings to address the key flaws in its Proposition 36 population estimates and adjust its population‑related funding requests at the May Revision accordingly. We recognize that any estimates will be subject to significant uncertainty due to the limited amount of actual data since the enactment of Proposition 36. However, the key flaws we identify above are conceptual problems that can be improved through reasonable assumptions in areas where actual data are lacking. We will continue to monitor CDCR’s populations and the other factors affecting the proposed adjustments and make recommendations based on the updated information available at the May Revision, including the administration’s revised population projections.
San Quentin Rehabilitation Center and The California Model
Background
Broad Framework for California Model Articulated by the Secretary and Receiver. On April 4, 2023 the Secretary of CDCR and the federal Receiver who oversees prison medical care issued a joint memorandum expressing their concern that prison environments can be unfavorable to the health and well‑being of the people who live and work in them and operate at cross purposes to rehabilitative efforts. To address this concern, they announced the department is implementing the California Model, which aims to make “system changes that create an environment rich in rehabilitation, a safer and more professionally satisfying workplace for all staff, and improve outcomes and opportunities for success through robust re‑entry efforts.” More specifically, the memorandum cited the following goals: (1) improving the health and well‑being of people who live and work in California prisons, with a focus on reducing trauma and toxic stress; (2) reducing recidivism; and (3) reducing incidents of use of force, staff assaults, overdoses, self‑harm, homicides, suicides, grievances, self‑isolation, and admissions to Mental Health Crisis Beds. In addition, the memorandum outlined four pillars intended to guide development of specific policy and practice changes:
- Dynamic Security. Dynamic security is an approach to security that promotes positive relationships between staff and incarcerated people through purposeful activities and professional, positive, and respectful communication.
- Normalization. Normalization involves bringing life in prison as close as possible to life outside of prison to make it easier for people to adjust to life in the community upon release. Normalization can involve changes to physical features (such as adding furniture that more closely mirrors furniture used outside prison) or changes to experiences, routines, or interactions (such as celebrating cultural events).
- Peer Support. Peer support involves training incarcerated people to use their lived experiences to provide recovery and rehabilitative support to their peers.
- Trauma Informed Organization. Becoming a trauma informed organization involves changing the practices, policies, and culture of the department to recognize the impacts of trauma and ensure the physical and emotional safety of all staff and incarcerated people.
Planning and Implementation Team Responsible for Developing the California Model Statewide. A planning and implementation team within CDCR is responsible for overseeing identification and implementation of the specific activities that align with the above goals and pillars. This team includes decision‑level representatives from all areas of the department and reports to an executive steering committee co‑chaired by the Secretary and Receiver.
Several Activities Are Being Implemented at Various Prisons. Below, we provide an overview of some of the primary activities that the department reports implementing to date. We note that some of these activities build on work that had already been under way for several years. In addition, these activities have largely been done without requests for additional resources.
- Resource Teams. Based on a model developed in Norwegian prisons, “resource teams” aim to reduce isolation and violence for the highest‑risk, highest‑need people in prisons. Officers on resource teams receive specialized training on the nature of mental illness and trauma, de‑escalation techniques, and strategies for motivating people to engage in rehabilitative programming and mental health care. These officers lead a team, including medical and mental health staff, to develop individualized plans to support out‑of‑cell time and engagement in positive activities while ensuring safety.
- Peer Support Specialist Programs. CDCR has launched various certified peer support specialist training programs through which people can learn to work as peer support providers while in prison. For example, peer support specialists can help with alcohol and drug recovery, navigating health care systems, teaching people how to advocate for themselves, and promoting self‑care. Peer support specialists receive certification and work experience while in prison that can potentially help them gain employment in a similar field upon release.
- Honor Dorms. CDCR operates certain housing units as “honor dorms,” which provide privileges and greater access to education and other programming in exchange for positive behavior. For example, a program at Valley State Prison in Chowchilla clusters people under age 26 where they are provided with enhanced programming opportunities and older incarcerated people who serve as mentors through one of the peer support specialist programs discussed above.
- Staff Training. CDCR has been rolling out staff training on California Model‑related topics, such as dynamic security and recognizing and responding to the impacts of trauma. In addition, the department reports that it is in the process of adapting its 13‑week Basic Correctional Officer Academy to reflect the California Model.
- Normalization Efforts. CDCR reports various efforts to change physical spaces in prisons, such as by incorporating more comfortable, home‑like furniture and bedding as well as adding gardens and murals. In addition, prisons have been encouraged to look for opportunities to bring elements of normal life into prison—such as graduation ceremonies, music events, and barbeques—sometimes inviting loved ones of incarcerated people into the prison to participate.
Department Has Identified Certain Metrics to Measure California Model Impacts. The California Model planning and implementation team indicates that it is tracking data related to drug overdoses, self‑harm, misconduct, rehabilitative program participation, and post‑release connection services as a starting point for measuring the impacts of the California Model. The department is expecting to see reductions in violence, use of force, and allegations of staff misconduct.
Governor’s San Quentin Advisory Council Recommended Changes for San Quentin Rehabilitation Center (SQRC). In May 2023, Governor Newsom convened an advisory council to recommend changes at SQRC in line with the California Model framework as a pilot to potentially be scaled up. In January 2024, the advisory council released a report containing 44 recommendations. Many of these recommendations differ from, or go beyond, the activities being implemented under the oversight of the California Model project and implementation team. For example, the report recommended single‑celling the entire prison, which would involve reducing the population of the prison. It also recommended creating a new job role called a “community correctional officer” for select correctional officers at SQRC who apply to receive enhanced training in how to support rehabilitation.
2023‑24 Budget Act Authorized Construction of a New Learning Center at SQRC. The 2023‑24 Budget Act authorized $360.6 million (subsequently reduced to $239 million as recommended by the advisory council) in lease revenue bond authority for the construction of a new learning center at SQRC, which is expected to be completed in early 2026. The center will contain 28 classrooms (nearly triple the existing classroom space at the prison) a library, a media center, staff offices, a large multipurpose gathering space, a café, and a store.
California Model Project and Implementation Team and Advisory Council Leadership Working to Identify Next Steps for SQRC. The California Model project and implementation team reports that it is currently working with leaders of the San Quentin advisory council to review each of the advisory council’s recommendations and identify those that have already been implemented and those that will be pursued in the future. This analysis is expected to be completed sometime this spring. In addition, the project and implementation team indicates that after identifying the recommendations that will be pursued, it plans to engage stakeholders at the prison—such as rehabilitative program providers—in workgroups for further planning activities.
Governor’s Proposals
The Governor proposes a total of $7.8 million General Fund and 33.6 positions in 2025‑26 (increasing annually to $13 million and 74.4 positions by 2027‑28) to (1) activate the new learning center, (2) contract with the American Job Center of California (AJCC), and (3) make various programmatic enhancements. We discuss these elements of the proposal in more detail below.
Activate the New Learning Center ($6.2 Million Ongoing by 2027‑28). The proposal includes $3 million in 2025‑26 (growing to $6.2 million in by 2027‑28) to support the operation of the new learning center. At full implementation, this would include 24.8 custody positions, 8 plant operations positions, 5 information technology positions, 2 librarian positions, and 1 position to support community engagement (such as by processing security clearances for volunteers to enter the prison).
Contract With AJCC ($200,000 Ongoing). The proposal includes $200,000 ongoing to partner with AJCC, which provides one‑on‑one career counseling and job placement assistance for people nearing release from prison. The proposal assumes AJCC would assist approximately 1,200 people at SQRC annually.
Make Various Programmatic Enhancements ($6.6 Million Ongoing by 2027‑28). The proposal includes $4.6 million in 2025‑26 (growing to $6.6 million by 2027‑28) to make the following expansions to custody staffing and rehabilitative programming capacity:
- Provide Additional Custody Staff for Existing Areas of the Prison. The proposal includes 21.6 custody positions, which would be assigned to housing units to engage with residents to build trust, rapport, and help them navigate rehabilitative opportunities at the prison.
- Expand Basic and Secondary Education Capacity. The proposal includes eight teacher positions, which would allow CDCR to expand basic and secondary education capacity by 432 students, roughly doubling capacity.
- Establish Bachelor’s Degree Program. The proposal includes funding and two positions to contract with a college to establish a bachelor’s degree program at SQRC to serve 140 students at full implementation. This would be in addition to two existing associate degree programs currently offered at SQRC. CDCR currently has bachelor’s degree programs at 10 other prisons with a total of about 400 students.
- Establish Electrical and Barbering/Manicurist Training Programs. The proposal includes two positions and funding for start‑up costs to establish two new career technical education (CTE) programs—serving a total of 54 new students—in the space that will be vacated by existing rehabilitative programs that are relocated to the new learning center. The administration indicates that it selected electrical and barbering/manicurist programs based on employment trend data. Current CTE programs at the prison are plumbing, painting, and machine shop and can serve a total of 81 students.
Assessment
Resources to Activate New Building Appear Reasonable. We find that it is reasonable to provide the custody and other support staff that would enable SQRC to activate the new learning center after construction is completed. Doing so would allow rehabilitation programs that already exist at the prison to move into the new building designed for them and for people to begin accessing the library and other common areas in the building.
AJCC Contract Appears Reasonable. We find that it is reasonable to contract with AJCC to provide job counseling and placement services at SQRC given that such services could help people find employment after release and the cost of the contract is relatively small.
Administration Has Not Developed a Clear Plan for SQRC. As discussed above, the California Model project and implementation team—and the administration more broadly—is still in the process of reviewing the San Quentin advisory council’s recommendations to determine which ones it will pursue. In addition, once it determines which to pursue, it will need to identify a clear strategy and action plan for achieving those recommendations, many of which articulate a vision but do not specify the actual steps needed to achieve it. For example, the advisory council recommends creating a rehabilitation and reentry plan for every person that reflects their healthcare, education, job training, recreational, and other rehabilitative needs and goals. To effectively pursue this goal, CDCR would need to review its existing resources and processes for rehabilitation and reentry planning, determine how and why they are falling short of the advisory council’s vision, and identify the specific resources and/or process changes that are necessary to overcome those barriers. Moreover, while the project and implementation team indicates it intends to engage key stakeholders at the prison—such as rehabilitation program providers—it has not yet done so. In sum, at this time, the administration has not (1) determined which pieces of the advisory council’s vision it wants to pursue; (2) prepared a strategy and specific action plan to pursue that vision; or (3) vetted the plan with key stakeholders, many of whom will be critical to implementing it.
Premature to Approve Remainder of Request Until SQRC Planning Process Has Been Completed. Because the administration has not yet completed its planning process for SQRC, we find that it is premature to approve the remaining portions of the request. Below, we discuss these portions of the request and why certain critical pieces of planning are necessary before the Legislature can determine if they are worth pursuing relative to its other budget priorities.
- Custody Staff Not Associated With the New Learning Center. The proposal includes 21.6 custody positions that would primarily be assigned to housing units to engage with the population. The department has provided high‑level descriptions of the job duties for these positions. However, it is unclear how these staff and their duties would fit into the administration’s overall plan for SQRC because one has not yet been developed. For example, a portion of these staff would be required to “collaborate with the California Model team to support rehabilitative programming, through feedback and observations made in the housing units.” However, the department has not provided any details on this California Model team, including who it consists of and what its role is. The lack of clarity on these positions is particularly notable given that they could represent a relatively high resource commitment if scaled up. Specifically, at a $3.6 million annual cost for SQRC alone, this additional staffing could cost around $100 million annually to implement statewide—particularly notable given the multiyear deficits facing the state.
- Basic and Secondary Education Capacity Expansion. CDCR reports that it is in the process of developing criteria for who will be housed at SQRC with a focus on maximizing the number of people who will be able to take advantage of the enhanced rehabilitation opportunities at SQRC. Accordingly, the makeup of the population that will be housed at SQRC is not yet clear. This makes it unclear whether the proposed expansion of basic and secondary education capacity is needed. For example, if the makeup of the population shifts toward people who have a demonstrated history of participating in programs, they may be more likely to have completed basic or even secondary education by the time they reach SQRC. This is probable because people are generally required to meet certain basic education requirements before they can participate in some rehabilitation programs.
- New Bachelor’s Degree Program. The administration has not provided data showing a demand for additional bachelor’s degree program capacity systemwide. Accordingly, it is unclear whether adding a bachelor’s degree program at SQRC would simply siphon some of the roughly 400 bachelor’s degree students off of existing bachelor’s degree programs at other prisons or whether it would actually result in more bachelor’s degree attainment. In addition, Mount Tamalpais College—a private accredited college based at SQRC—currently offers an associate’s degree program and operates entirely through private philanthropy. It may be possible that Mount Tamalpais College could expand its associate’s degree capacity—or add a bachelor’s degree program if the demand indeed exists—at no cost to the state. However, because the administration has not yet engaged stakeholders in developing a specific plan, it is unclear if this option was considered. Moreover, SQRC has many other existing nonstate‑run rehabilitation programs. It is possible that after conducting its stakeholder engagement process, it will determine that some of those programs represent a higher priority for expansion than adding a new bachelor’s degree program.
- New Electrical and Barbering/Manicurist Training Programs. Because the policies that will impact the makeup of the population at SQRC have not yet been finalized and the department has not yet engaged stakeholders in the planning process, it is unclear whether electrical and barbering/manicurist programs represent the highest priority for expansion at this time.
Key Questions Remain Unanswered for the California Model as a Whole. Even after the administration develops a specific plan for SQRC, certain key questions will remain about the California Model as a whole. Without answers to these questions, it is difficult for the Legislature to provide oversight over the development and implementation of the California Model and evaluate any future funding requests. We discuss these key questions below.
- How Is Progression Through the Prison System Envisioned? Several of the activities being piloted under the California Model are targeted toward specific populations and environments within the prison system. For example, resource teams are typically focused on some of the most challenging populations in the highest‑security environments in the system. In addition, honor dorms—at least as they have been implemented so far—seem to be focused on specific subpopulations, such as people under the age of 26. However, the administration has not articulated how these various interventions fit together to motivate behavior change in a continuum through the prison system from admission to release. Without a clear theory of action, it is difficult to assess the overall logic of the activities being pursued under the California Model and to identify any potential gaps. For example, of the roughly 30,000 people released from prison annually, roughly half spend around a year or less in prison. A clear theory of action would articulate how the California Model would better serve this large group with short stays and what specific outcomes we might logically expect to see as a result.
- What Is the Role of SQRC in the Envisioned Progression? The ongoing construction and current request for operational funding at SQRC are substantially more costly than California Model activities being implemented at other prisons. Moreover, the administration has indicated an intention to single‑cell SQRC, which would reduce the number of people that can otherwise be housed at the prison, thereby concentrating the richer resources at SQRC among an even smaller number of people. Given this resource intensity, the pilot project being developed at SQRC requires a higher level of scrutiny. In particular, the administration should be able to articulate how SQRC fits into its overall theory of action for the entire prison system and why it would logically contribute to the administration’s stated outcomes. For example, if the administration believes that access to single‑celling and richer programming will motivate people at other prisons to make more positive choices in the hopes of being placed at SQRC, then it should explain how it believes this incentive would function. For example, how would people at other prisons learn of the benefits of SQRC? What are the intermediate positive steps and institutional responses that would mark someone’s pathway to SQRC?
- How Would the Administration’s Vision Be Implemented? After establishing a theory of action for how the California Model could logically lead to its stated goals, the administration should identify the key policy changes and additional budget capacity that it would need to implement this vision. For example, if the administration aims to offer single‑celling more broadly throughout the prison system, then it would need to articulate a specific plan to either expand prison capacity (which could be very costly) or reduce the prison population sufficiently to achieve its desired level of single‑celling. While it may be premature for the administration to know specific implementation details, it should be able to articulate the broad contours of a plan at this point. If it cannot do so, this raises concerns that the administration’s vision is not feasible to implement. Moreover, even if the Legislature agrees with the administration’s vision, it will want to ensure that it is comfortable with the steps and budgetary resources that would be required to achieve it. Given the multiyear deficits facing the state, it is particularly important that the Legislature understands the fiscal implications of the administration’s plans so that it can weigh California Model activities against its other budget priorities.
- What Would Success Look Like? Based on its theory of action and high‑level implementation plan, the administration should be able to articulate how it would know if the model is working as expected. Specifically, the department should be able to articulate how the metrics it is tracking would logically be affected by the California Model and how it would know if trends in those metrics are indeed caused by the California Model as opposed to other factors. For example, one goal could be to reduce violence at SQRC. However, simply measuring the number of violent incidents at SQRC before and after the pilot is implemented would not be a clear indicator of success because the department is planning to change the makeup of the population of the prison, which could affect violence levels independently of the other changes being developed. In contrast, if the administration believes that SQRC will help motivate positive behavior change throughout the system, then perhaps the degree to which people report actively working to earn transfer to SQRC and the number that are successfully transferring there from higher‑level institutions could be an indicator of success.
- How Will Success Be Measured and Evaluated? After it has a clear sense of what success would look like under its theory of action, the administration should develop a detailed plan for measuring and evaluating whether success is being achieved. Such a plan would include a description of the specific data points and benchmarks that will be used to measure progress. To the extent certain needed data are not currently collected, the plan would identify how that data will be collected, including the instruments or counting rules that will be used to gather it, the data systems that will be used to manage it, and the staff responsible for doing this. In addition, such a plan would identify who will evaluate data to assess if benchmarks are being met and report on the results. Given that the California Model touches on many areas of the department and has wide ranging goals, an evaluation plan may involve several components and entities. For example, it could make sense to contract with external researchers to survey staff and evaluate whether metrics of staff wellness are improving. In contrast, it could make sense for state entities that already play a role in oversight of CDCR—such as the Office of the Inspector General or the California State Auditor—to monitor implementation of or adherence to new policies.
Recommendations
Approve Resources to Activate New Learning Center and Contract With AJCC. We recommend that the Legislature approve the portions of the request to activate the new Learning Center and contract with AJCC. This would allow existing programs at the prison to begin utilizing the space and for people preparing to reenter the community to receive career counseling and job placement services. This would be a total of $3.2 million and 19.7 positions in 2025‑26, growing annually to $6.4 million and 40.8 positions by 2027‑28.
Reject Remaining Resources Unless Administration Is Able to Provide a Clear Plan for SQRC Justifying Them. In view of the above concerns, we recommend that the Legislature only approve the remainder of the request if the department is able to provide a complete action plan for SQRC that is consistent with legislative priorities and justifies the requested resources.
Require Administration to Report on Key Unanswered Questions. We recommend that the Legislature adopt budget bill language requiring the administration to submit a report by January 10, 2026 that answers the key questions outlined above. We note that the Legislature may want to explicitly direct the department to engage with stakeholders as it develops answers to these questions. To the extent that the administration cannot fully answer these questions by January 10, 2026, the report should outline the process for and time frame in which the questions will be answered.
Inpatient Mental Health Beds
Background
Overview of CDCR Mental Health. All people entering the prison system are screened for mental health needs. About one‑third of the prison population has a diagnosed mental health need. The mental health care provided at the prisons is subject to the oversight of a Special Master appointed as part of the Coleman v. Newsom federal court case, which ruled in 1995 that CDCR was not providing constitutionally adequate mental health care. Most people in prison with a mental health need can be treated in an outpatient setting, meaning they live in a prison housing unit and receive regular mental health treatment but do not require 24‑hour care. However, under certain circumstances, some people may require more intensive treatment provided in an inpatient bed. These inpatient beds provide intensive 24‑hour care with the goal of preparing the people to return to an outpatient program. Below, we discuss the various types of inpatient beds provided at CDCR.
CDCR Operates Mental Health Crisis Beds (MHCBs) to Address Shorter‑Term Acute Needs. If people are suffering from severe symptoms of a serious mental health need that cannot be managed by an outpatient program, they are generally sent to MHCBs, which provide short‑term housing and 24‑hour care. Due to their immediate need for treatment, people referred to MHCBs are supposed to be transferred to these beds within 24 hours. When an MHCB is unavailable at a specific prison, CDCR typically transports people to another prison with an available MHCB. Under CDCR regulations, people are not supposed to stay in MHCBs for more than ten days. The annual cost of operating each MHCB is around $400,000—including custody staff. Currently, there are 392 MHCBs at men’s prisons and 41 MHCBs at women’s prisons. Normally, MHCBs must be licensed by the California Department of Public Health to ensure compliance with minimum standards established for patient safety and quality of care. However, 53 of the MHCBs in CDCR are unlicensed and are legally allowed to operate only due to a waiver from the Coleman court. Most of the state’s unlicensed MHCBs are in a 34‑bed facility operated at the California Institute for Men (CIM) in Chino.
CDCR Uses Other Types of Inpatient Mental Health Beds for Longer‑Term Needs. If a patient’s condition is stabilized in an MHCB, the patient is generally sent back to a housing unit. However, if the patient’s condition requires longer‑term, 24‑hour care, the patient may be admitted to inpatient beds designed for such care. In prison, these beds are operated by CDCR. However, patients may also be placed in such beds in a state hospital operated by the Department of State Hospitals (DSH) through a referral process. There is a total of 1,632 of these beds—1,296 in prisons and 336 in state hospitals. These beds are divided into the following two types based on the nature of the care they provide:
- Acute Psychiatric Programs (APPs). APPs provide shorter‑term, intensive treatment for people who show signs of a major mental illness or higher‑level symptoms of a chronic mental illness. Patients are supposed to be transferred to an APP within 72 hours of the referral, but no more than ten days after the referral and can generally stay up to 45 days. Currently, there are 489 APP beds, all of which are in state prisons. The annual cost of operating one of these beds is $300,000.
- Intermediate Care Facilities (ICFs). ICFs provide care beyond what is provided in CDCR outpatient programs, but are available for longer time periods than MHCBs or APPs. People with lower security concerns are placed in low‑custody ICFs, which are in dorms, while those with higher security concerns are placed in high‑custody ICFs, which are in cells. There are 722 ICF beds in state prisons, 658 of which are high‑custody ICF beds. In addition, there are 306 low‑custody ICF beds in state hospitals which CDCR can refer patients to. Each ICF bed in a state prison costs around $246,000 annually to operate, while those in DSH cost around $393,000 annually.
The department also maintains 85 beds for women and people sentenced to death in state prisons that can be operated as either ICF or APP beds. Additionally, there are 30 beds in state hospitals that CDCR can refer women to. Due to the specific groups these beds serve, these beds are costlier to operate—about $364,000 annually.
CDCR Determines How Many Beds to Operate Based on Projections and Court Requirements. The number of beds CDCR operates are a part of a court‑required bed plan. The department determined how many beds to operate based on projections of the mental health population completed by a private contractor using a methodology approved by the federal court. These projections are updated biannually and used to develop a bed need study that compares the department’s mental health bed capacity with its current and projected mental health populations. The court requires CDCR to operate at least 10 percent more beds than the projections imply would be needed to act as a “buffer” against unexpected surges in bed need. (We note that the bed need study counts the 336 inpatient beds in state hospitals towards the prison inpatient capacity.) CDCR cannot modify the number of beds without notifying the Special Master and receiving approval from the Coleman court.
CDCR Is Constructing a Mental Health Crisis Facility at CIM to Reduce Unlicensed Beds and Transfer Time. Since 2017, the state has approved a total of $141.1 million ($7.5 million General Fund and $133.6 million lease revenue bond authority) to construct a 50‑bed mental health crisis facility at CIM. CDCR sought the project in order to (1) replace 34 unlicensed MHCBs at CIM with licensed beds and (2) reduce the amount of time it takes to transfer people in Southern California prisons to MHCBs by adding 16 MHCBs in the region. CDCR reports that, currently, a lack of MHCBs in Southern California forces it to transfer some people in Southern California prisons to Central and Northern California prisons where more MHCBs are available. The project at CIM is expected to be completed in October of 2025.
CDCR Is Being Fined for Failing to Fill Mental Health Positions. As part of the ongoing Coleman court case, CDCR has been incurring fines monthly since April 2023 for failing to reduce vacancy rates for five mental health classifications, which include: psychiatrists; psychologists; clinical social workers; recreational therapists; and medical assistants. Many of these positions are used to operate inpatient mental health beds. The Coleman court requires that each of the five classifications have a vacancy rate below 10 percent otherwise the state is fined for each classification out of compliance. The state has paid over $150 million in fines so far, which are deposited in a special account to support staff recruitment and retention. At the time of publication, CDCR is still accruing fines but the court has paused on collecting and spending the fines due to ongoing litigation.
Governor’s Proposal
Activation of Newly Constructed Mental Health Crisis Facility. The Governor’s budget proposes $3 million General Fund and 13.4 positions in 2025‑26, growing to $4.4 million and 20.4 positions in 2026‑27 and ongoing, to staff the 50‑bed mental health crisis facility at CIM. Additionally, the 34 unlicensed beds currently operated at CIM would be deactivated and the $16.4 million General Fund and 86.2 positions currently supporting these beds would be shifted to staff the new facility. Accordingly, CDCR would have a total of $19.4 million and 99.6 positions to staff the facility in 2025‑26, growing to $20.8 million and 106.6 position in 2026‑27 and ongoing.
Assessment
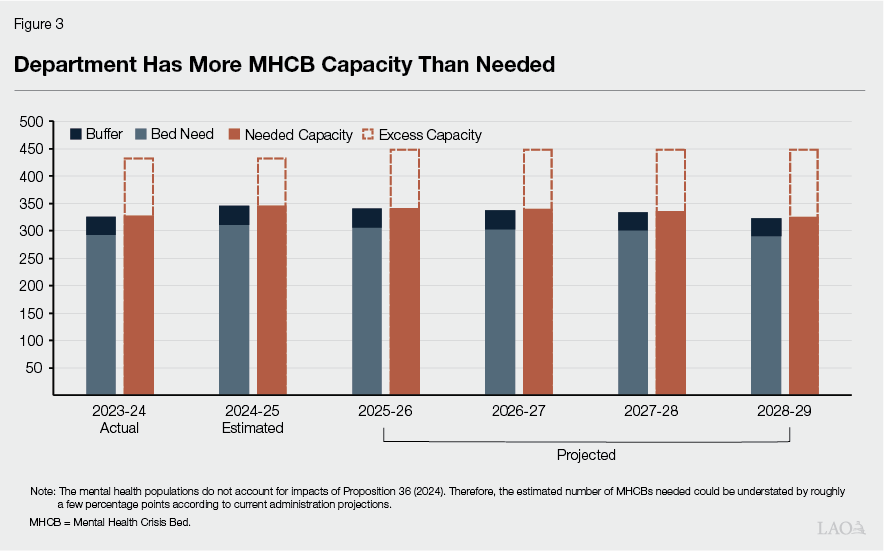
Activation of Mental Health Crisis Facility Would Increase Amount of Statewide Excess Capacity. The underlying rationale for the newly constructed facility still remains, as it would allow the department to convert its unlicensed beds to licensed beds and it would help address capacity limitations in the Southern California region, thereby reducing the number of people needing to be transferred to other parts of the state. However, while the new facility helps address regional capacity challenges, the department has excess MHCB capacity when viewed at the statewide level. As shown in Figure 3, with the added capacity provided under this proposal, the department will continue to have more than enough existing capacity to meet all of its current and projected needs for licensed MHCBs. CDCR needs 341 MHCBs systemwide in 2025‑26, but it is proposing to operate 449 MHCBs—an excess of 109 MHCBs (84 at men’s prisons and 25 at women’s prisons). Furthermore, CDCR’s MHCB needs are projected to decline by 25 additional beds by June of 2029. Based on this projection, excess capacity would rise to 134 beds. This does not account for the increase in the prison population caused by Proposition 36, which could also increase the mental health population. However, we anticipate that even after adjusting for the effects of Proposition 36 there will still be excess capacity. For example, if Proposition 36 increases the number of MHCBs needed by 4 percent in 2025‑26 (the amount the administration expects the measure to increase the overall population by in that year) there would still be 95 excess beds in 2025‑26. (The bed need study, as well as the projections of the prison population and the effects of Proposition 36, will be updated at the May Revision. For more information, please see the “State Prison and Parole Population and Other Biannual Adjustments” section of this brief.)
MHCB Proposal Does Not Account for Reduced Costs Related to Transfers. As discussed above, the new MHCB facility would likely reduce transportation costs, as fewer people in Southern California would need to be transferred to beds in more northern parts of the state. However, the Governor’s proposal does not account for these potentially modest savings.
CDCR Also Continuing to Operate Excess APP and ICF Bed Capacity. As shown in Figure 4, CDCR is also operating excess capacity in other types of inpatient beds, including 205 APPs, 327 ICFs at both men’s prisons and state hospitals, 32 APP/ICF beds at women’s prisons, and 13 APP/ICF beds for the condemned population. Similar to MHCBs, adjusting the population for Proposition 36 would somewhat reduce the amount of excess capacity in these beds, but the department would likely still be operating significantly more inpatient beds than needed.
Figure 4
Department Has More Acute Psychiatric Program (APP) and
Intermediate Care Facilities (ICF) Beds Than Needed
|
Proposed |
2025‑26 |
2029 |
||||
|
Projected Bed |
Excess |
Projected Bed |
Excess |
|||
|
ICFa |
1,028 |
702 |
327 |
667 |
361 |
|
|
APP |
489 |
285 |
205 |
271 |
218 |
|
|
Women’s prisonsb |
75 |
43 |
32 |
42 |
33 |
|
|
Condemned population |
40 |
27 |
13 |
25 |
15 |
|
|
Totals |
1,632 |
1,056 |
577 |
1,005 |
627 |
|
|
a306 of these beds are in state hospitals. z30 of these beds are in state hospitals. |
||||||
|
Note: Totals may not add due to rounding. |
||||||
Reducing Excess Capacity Would Create Savings and Help With Court Compliance. If the department were to reduce MHCB, APP, and ICF bed capacity, we estimate that this could result in annual ongoing savings ranging from tens of millions of dollars to more than $100 million, depending on the number of actual beds that are deactivated. The savings primarily would result from the elimination of hundreds of mental health positions needed to staff these beds. The reductions in staffing would have the added effect of reducing the vacancy rate of mental health staff. This would help the state comply with the Coleman court’s order to reduce mental health vacancies, likely allowing the state to reduce the amount of fines that would be levied on the state. As such, there could be additional significant fiscal benefits from rightsizing inpatient mental health bed capacity based on the projected need. As discussed earlier, CDCR would need to notify the Special Master and receive approval from the Coleman court to make changes in bed need capacity.
Recommendation
Approve Activation. We recommend approving the proposed activation of the CIM mental health crisis facility. Doing so would allow the department to convert unlicensed MHCBs to licensed beds. This could improve the quality of care provided by the state. Furthermore, it could reduce the time it takes to transfer people from the Southern California region to MHCBs.
Direct CDCR to Seek Approval to Align Inpatient Bed Capacity With Updated Bed Need Study. Given that CDCR’s estimates indicate there would be 686 excess inpatient beds—including MHCBs and other inpatient beds operated by CDCR and DSH—in 2025‑26, we recommend that the Legislature direct CDCR to seek approval from the Coleman court to reduce excess capacity as part of the May Revision. Specifically, we recommend directing CDCR to seek authorization from the Coleman court to include a proposal in the May Revision to reduce inpatient bed capacity based on a revised bed need study. To ensure excess capacity does not accumulate in future years, we further recommend that the Legislature add budget bill language requiring CDCR to regularly seek adjustments to its inpatient mental health bed capacity based on the bed need study. We anticipate these changes would reduce CDCR costs—both from operating the excess capacity and avoided fines—by potentially more than $100 million annually, if all the excess beds are approved for deactivation by the Coleman court. This would not only free up General Fund resources that could be used to address the multiyear deficits facing the state, but could help CDCR comply with the Coleman court order to reduce mental health vacancies. To the extent, the Coleman court denies a plan to deactivate excess bed capacity, it would benefit the Legislature to understand what criteria, threshold, or buffer the state would have to achieve under the Coleman court in order to deactivate some, if not all, of the excess capacity. The Legislature could consider having CDCR work with Special Master to produce such a report at that time.
Direct CDCR to Account for Transportation Savings. Because the MHCB proposal did not account for potential savings from transportation costs, we recommend that the Legislature also direct CDCR to include a proposal at the May Revision that accounts for such savings.
Suicide Watch
Background
CDCR Provides Intensive Short‑Term Monitoring to Prevent Suicides. When a person in prison is suspected of being a danger to themselves, CDCR policy requires that the person be provided with short‑term intensive monitoring. This monitoring—referred to as suicide watch—is typically conducted by health care staff on a one‑on‑one basis. Staff take shifts watching the person up to 24‑hours a day. The department has various positions that can perform this one‑on‑one monitoring, but generally starts with certified nursing assistants (CNAs). However, when a CNA is not available, the department assigns other staff. These other assigned staff, such as psychiatric technicians and registered nurses, are compensated at a higher rate, making suicide watch costlier when these classifications are used. Specifically, data provided by CDCR indicate CNAs cost about $42 per hour while the department spends an average of about $69 per hour when using other positions for this work.
CDCR Budget Includes Funding for Suicide Watch. Prior to the 2017‑18 budget, CDCR managed suicide watch workload within its existing resources by often redirecting correctional and healthcare staff and using overtime. However, as suicide watch hours increased, it became more challenging for the department to redirect resources and staff for suicide watch without negatively affecting other workload. In the 2017‑18 budget, CDCR received $3 million ongoing General Fund and 185 CNA positions for suicide watch workload. While the full cost of these position was around $12 million, at the time, CDCR indicated it could use preexisting funding in its budget for overtime and other costs to absorb the remaining $9 million cost of the suicide watch workload. Separately, the biannual population adjustment process provides additional funding for CNA positions based on the number of health care beds CDCR operates. Some of these CNAs can also be used for suicide watch, but the process does not make any specific adjustments to suicide watch staffing based on changes in population. The 2024‑25 budget provided CDCR with $3.8 million General Fund and a total of 197.5 CNA positions for suicide watch. If combined with the $9 million in costs CDCR reports it has typically absorbed for suicide watch workload, total resources for suicide watch in 2024‑25 are about $12.8 million.
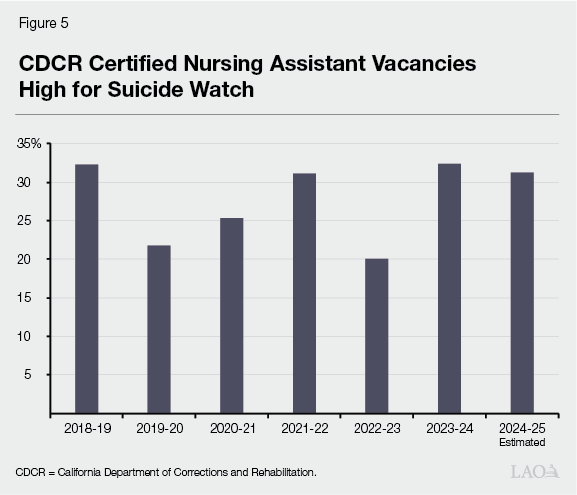
CDCR Has Experienced Notable CNA Vacancy Rates for Suicide Watch, but Has Had Success Hiring CNAs More Recently. Vacancy data reported by the department show that nearly one‑third of CNA positions for suicide watch—about 60 positions—are currently vacant. Although there have been fluctuations in vacancy rates in prior years, Figure 5 shows that the CNA vacancy rate has remained between 20 percent and 32 percent. This is relatively high compared to the statewide vacancy rate for all employees, which was 18 percent in December 2024. These trends suggest that the department has struggled to fill these positions in recent years. However, it is possible that this could change going forward. For example, the department indicated that, as of January 2025, it was in the process of hiring 79 CNAs from one recruitment event.
Department Consistently Overspends Budget. CDCR reports that, due to the frequent need to use positions other than CNAs for this work, they have routinely overspent their budget. As shown in Figure 6, CDCR has spent about $31 million on suicide watch annually and projects to spend about the same in the current year, resulting in overspending by $18.4 million. When overspending occurs, CDCR has to redirect funding in its budget—such as savings from unfilled positions elsewhere in the department—to cover these costs. However, CDCR reports that it can no longer redirect this level of resources.
Figure 6
CDCR Consistently Spends More Than Budgeted
on Suicide Watch
(In Millions)
|
2020‑21 |
2021‑22 |
2022‑23 |
2023‑24 |
2024‑25a |
|
|
Authorized expendituresb |
$12.9 |
$12.8 |
$12.8 |
$12.8 |
$12.8 |
|
Actual expenditures |
30.3 |
31.6 |
29.2 |
33.7 |
31.2 |
|
Difference |
‑$17.4 |
‑$18.8 |
‑$16.4 |
‑$20.9 |
‑$18.4 |
|
aEstimated. bIncludes $9 million in costs that the department has historically absorbed. |
|||||
|
CDCR = California Department of Corrections and Rehabilitation. |
|||||
CDCR Exploring Alternatives to Supplement Suicide Watch Hours. CDCR has indicated that it plans to work with the Coleman court and the California Department of Human Resources to identify a different classification for suicide watch that can supplement CNA positions. (As discussed in greater detail in the “Inpatient Mental Health Beds” section of this brief, the Coleman court is a federal court that oversees the provision of mental health care in CDCR pursuant to a lawsuit known as Coleman v. Newsom.) According to the department, the identified classification could cost more than CNAs but would cost less than the other positions CDCR uses for suicide watch, reducing the number of hours that the higher‑cost positions currently provide. CDCR also anticipates that this additional classification would be easier to fill than CNAs.
Governor’s Proposal
Suicide Watch Augmentation. The Governor’s budget includes a $13.6 million General Fund augmentation in 2025‑26 and ongoing to fund costs associated with suicide watch workload. This would bring total budgeted resources for suicide watch to $17.4 million annually. The requested amount reflects that CDCR reports it can continue to absorb $9 million on an ongoing basis as well as an additional $5 million of suicide watch workload—for a total of $14 million annually. As such, the total resources for suicide watch would be $31 million on an ongoing basis. Notably, CDCR is not requesting additional positions. Instead, the requested funds would largely pay for using more costly positions when CNAs are unavailable.
Assessment
Proposed Funding May Be More Than Needed… Under the Governor’s proposal, CDCR would receive an ongoing amount of funding that reflects the costs of redirecting more expensive positions to suicide watch. However, there are a couple of reasons to think the full $13.6 million requested by CDCR might not be necessary to pay the future costs of suicide watch. First, CDCR reports hiring 79 CNAs in a single hiring event in January 2025 as mentioned above. This suggests CDCR is experiencing greater success in reducing the CNA vacancy rate, which would reduce the cost of suicide watch. For example, if CDCR successfully fills all of its vacant CNA position, these lower‑cost positions could reduce the annual cost of suicide watch by about $2.8 million. Second—even if CDCR cannot maintain its success in recruiting CNAs—costs could be lower if the department is successful in its efforts to identify a classification that is easier to fill and has a lower cost than some of the positions that are currently used.
…And Would Not Adjust to Changes in Suicide Watch Workload. Currently—and under the Governor’s proposal—CDCR receives more or less a set amount of funding for suicide watch irrespective of changes in the size of the population. However, it is possible that suicide watch hours could increase or decrease in the future with changes in the prison population. For example, data published by CDCR show that nearly two‑thirds of suicide decedents had a mental health designation in 2023, and nearly 90 percent in 2022. To the extent there are changes in the population at risk of suicide, it could drive changes in suicide watch workload. If the number of suicide watch hours needed declines, then the department would be overfunded for these services. On the other hand, if the number of suicide watch hours were to increase, CDCR would be underfunded and likely be forced to use higher‑cost positions rather than CNAs because of its limited position authority.
Recommendation
Approve One‑Time Funding. Because suicide watch is critical to patient safety and the department has struggled to fill these positions in recent years, we recommend the Legislature approve the proposal on a one‑time basis. However, the ongoing costs of suicide watch are still uncertain as there are reasons to think it might decline in the future—particularly if CDCR takes steps we recommend below to reduce costs. Limiting the funding to one‑time would give the Legislature a natural opportunity to reassess the ongoing level of funding needed for suicide watch as part of the 2026‑27 budget process, and allow the department time over the next year to implement the steps we recommend below.
Direct CDCR to Take Steps to Reduce Costs of Suicide Watch. In order to reduce the costs of suicide watch and more closely track changes in workload, we recommend the Legislature direct CDCR to take the following steps:
- Continue Efforts to Fill CNA Vacancies. As noted above, if the department was fully staffed it could provide more suicide watch hours at a lower cost. As a result, we recommend the Legislature direct CDCR to continue to make efforts to fill the vacant positions. The recent success in hiring CNAs suggests the department may be successful in reducing the number of vacant CNA positions for suicide watch.
- Create Alternative Classification for Suicide Watch. We recommend that the Legislature direct CDCR to create an alternative position classification for suicide watch that can supplement the use of CNAs for this workload to the extent it cannot hire a sufficient number of CNAs to fully address this workload. CDCR should strive to identify a classification that is both (1) lower cost than the average the department has historically spent per hour on suicide watch by using other positions and (2) easier to recruit than CNAs.
- Direct CDCR to Develop a Population‑Driven Budgeting Methodology for Suicide Watch. We recommend the Legislature direct CDCR to develop a budgeting methodology for suicide watch that accounts for changes in the population that drive suicide watch hours. For example, CDCR could annually estimate its need for suicide watch based on the projected size of the overall population and/or portions of the population that are likely to contribute to suicide watch workload—such as people in prison with identified mental health needs. This would ensure the annual resources for suicide watch are more closely tied to the department’s needs—an especially important consideration given that the projected decline in the population will likely drive a decline in suicide watch workload.
To help the Legislature ensure that CDCR is making adequate progress on these steps, we recommend directing the department to report on (1) the strategies it is using to fill vacant CNA positions and data on the effectiveness of these strategies; (2) what classifications it is considering to use for suicide watch as an alternative to CNAs, the rationale for using such classifications, whether it continues to need an alternative to CNAs for suicide watch, and when it expects a new classification could be deployed; and (3) details on a population‑based budgeting methodology. This report should be provided to the Legislature no later than January 10, 2026. This would allow the Legislature to consider the report as it is determining the ongoing funding level for suicide watch as part of the 2026‑27 budget process.
Parole Community Rehabilitation Programs
Background
People on Parole Receive Services Through CDCR‑Funded Rehabilitation Programs
Certain People Released From Prison Are Supervised by CDCR on Parole. When people are released from prison, they are generally supervised in the community for a period of time—usually between one to two years. While some of these people are supervised by county probation departments, people convicted of a serious or violent offense are generally supervised by state parole agents. Alongside supervision, the state provides people on parole with access to a variety of rehabilitation services in order to successfully reintegrate them into the community. As noted in the “State Prison and Parole Population and Other Biannual Adjustments” section of this brief, CDCR projects there to be an average daily population of about 34,700 people on parole in 2025‑26.
CDCR Uses Contracts to Provide Rehabilitation Services to People on Parole. CDCR funds a number of different rehabilitation programs for people on parole throughout the state. These services are generally provided by contractors. Programs are structured as either residential programs that provide housing—typically paired with other services—or as programs that participants attend for a period of time during the day. These programs can last for months. For example, many last for up to 180 days but can be extended for an additional 185 days. Within these programs, people can receive various services such as substance use disorder (SUD) treatment, case management, sex offender treatment, and employment assistance. The revised 2024‑25 budget includes $233.9 million total funds for these programs, including $191.1 million from the General Fund. Below, we provide details on some of the key programs offered to people on parole.
- Specialized Treatment for Optimized Programming (STOP) Provides SUD Treatment and Housing. STOP is a CDCR‑funded program that provides a range of services to people on parole, but primarily focuses on various types of SUD treatment. These include residential and outpatient services but exclude Medication Assisted Treatment (MAT). (MAT combines SUD treatment services—such as cognitive behavioral therapy, a type of therapy which helps change negative patterns of behavior—with medications designed to reduce the likelihood of people relapsing while undergoing treatment.) CDCR currently has agreements with nonprofit and private contractors that administer STOP in six regions throughout the state. These regional STOP contractors (1) pay local STOP network providers to deliver services through subcontracts, (2) connect people with these providers, and (3) conduct oversight of the services provided. In 2024, the STOP network provided services to about 8,600 people on parole.
- Day Reporting Centers (DRCs) Connect People to Various Services. DRCs offer a “one‑stop shop” for people on parole to be connected to various nonresidential services, some of which are offered on site. The programs generally focus on addressing factors that might contribute to future criminal activity such as anger management, but also have a limited ability to connect people with transitional housing. There are 17 DRCs throughout California that served about 4,500 people in 2023‑24.
- Long‑Term Offender Reentry and Recovery (LTORR) Provides Housing and Services. LTORR programs are substance‑free, residential programs that provides housing, meals, and various services. The services generally focus on the needs of people that have served long prison sentences such as employment and computer‑supported literacy. There are 14 LTORR programs throughout California that served about 1,700 people in 2023‑24.
- Returning Home Well (RHW) Program Provides Housing Services on a Limited‑Term Basis. The 2022‑23 budget included $10.6 million annually for three years for the RHW program to provide emergency transitional housing services to people on parole. To implement the program, STOP contracts were amended to include additional housing‑only services. The RHW program serves people for a maximum of 180 days or 6 months. In 2023‑24, the RHW program served a total of about 1,500 people. The department is required to submit a report by March 1, 2026 that presents metrics and outcomes associated with the program.
State Has Started Providing Cost‑of‑Living Increases for Some Providers. As discussed in our publication The 2023‑24 Budget: Considering Inflation’s Effects on State Programs, inflation can erode the quantity and quality of state services, such as service obtained through contracts. For example, CDCR has indicated that in recent years there has been a lack of providers willing to bid on expired CDCR contracts because contract rates did not have cost‑of‑living increases built into them, meaning they have not kept up with increased costs resulting from inflation. It is possible that, rather than providing service to the state, these providers are instead servicing others, such as people referred by counties and private individuals. CDCR reports this has made it difficult to continue to provide services. To address this, the 2024‑25 budget provided several parole rehabilitation programs whose contracts were set to expire with a $2.3 million General Fund increase in 2024‑25 and an ongoing 2 percent annual cost‑of‑living increase thereafter. This funding provided cost‑of‑living increases specifically to five DRCs and six LTORR programs.
People on Parole Can Receive Certain Services Outside of CDCR‑Funded Programs
Medi‑Cal SUD Treatment Programs Are Available to Treat People on Parole. Some people on parole—particularly those receiving MAT—receive SUD treatment services outside of CDCR’s contracts. Usually, these services are funded through Medi‑Cal, the state’s Medicaid program, which provides health care coverage for low‑income Californians and is overseen by the state Department of Health Care Services (DHCS). Medi‑Cal SUD treatment services are administered locally by county behavioral health departments. Under the Medi‑Cal billing structure, counties receive a fee‑for‑service reimbursement for behavioral health services based on an established fee schedule. Counties then negotiate payment terms and rates for the provision of services with providers. Federal reimbursements rates range from 50 percent to 90 percent depending on various factors such as income, services received, and whether the person has dependent children. Most people being released from prison qualify for Medi‑Cal and are therefore eligible for these services. CDCR screens people before release and, as of 2023‑24, submits Medi‑Cal applications for about 83 percent of people released, while the remainder did not have applications submitted for various reasons, such as having access to other insurance or refusing service. Between July 2023 and June 2024 (the most recent data available), Medi‑Cal applications were submitted for about 24,900 people who were released. Of these applicants, about 20,100 (81 percent) were approved, 35 (less than 1 percent) were denied, and the remaining 4,800 (16 percent) were pending at the time of release.
State Is Expanding Housing Services Offered Through Medi‑Cal. The California Advancing and Innovating Medi‑Cal (CalAIM) initiative is a large set of reforms in Medi‑Cal to expand access to new and existing services and streamline how services are arranged and paid. Under CalAIM, DHCS has been implementing two new Medi‑Cal benefits targeted at the subset of Medi‑Cal beneficiaries with the most complex care needs. These complex care needs include issues related to homelessness. Notably, several housing‑related services—such as housing navigation services and term‑limited payments for housing (such as for security deposits or first month’s rent)—are included in CalAIM as optional benefits and have been implemented by at least one Medi‑Cal managed care plan in all 58 counties. (Over 90 percent of Medi‑Cal beneficiaries are enrolled in Medi‑Cal managed care plans, which are responsible for arranging and paying for most Medi‑Cal services on behalf of their members.) Recently, DHCS received federal approval to provide transitional rent to eligible Medi‑Cal members and draw down federal funding. The transitional rent service covers up to six months of rent for certain people including those transitioning into the community from correctional facilities or transitioning from homelessness. The benefit will be mandatory to provide for certain beneficiaries beginning January 2026, and mandatory for all eligible people beginning January 2027—though these services can be offered now. Similar to Medi‑Cal SUD treatment, between 50 percent and 90 percent of the cost of these services will be covered by federal reimbursements.
Governor’s Proposal
Build in Inflation Adjustments to Parole Rehabilitation Program Funding. The Governor’s budget proposes $32 million General Fund in 2025‑26, $34.6 million in 2026‑27, $37.3 million in 2027‑28, $40.1 million in 2028‑29, $42.9 million in 2029‑30, and ongoing increases annually thereafter to reduce the impact of inflation on parole rehabilitation programs. This consists of (1) a roughly 30 percent one‑time catch‑up adjustment and (2) an ongoing 2 percent annual cost‑of‑living increase for two DRCs, six LTORR programs, and all STOP contracts. The one‑time catch‑up adjustment is calculated based on when the service was first provided in each county and the cost‑of‑living increases that have occurred in that area since. The administration is proposing this catch‑up adjustment because the department has not increased funding in previous years for these contracts and is concerned that it will not receive any bidders on these contracts as previously happened at two locations with expired contracts. Of the total:
- $3.7 million in 2025‑26 (increasing to $5.1 million by 2029‑30 and growing annually thereafter) would be allocated to the DRCs and LTORR programs.
- $28.3 million in 2025‑26 (increasing to $37.8 million by 2029‑30 and growing annually thereafter) would be allocated to STOP contracts.
Extend Funding for RHW Program for Additional Two Years and Add Services. The Governor’s budget also includes $12.9 million General Fund in 2025‑26 and 2026‑27 to extend RHW for an additional two years and add services not currently provided, such as SUD treatment assessment and programming. This consists of $10.6 million in each year to maintain the existing housing program and $2.3 million to support additional nonhousing services for the RHW population, such as services related to SUD treatment and anger management. The department indicates that the additional services are necessary because people in the RHW program have an assessed need for these services. The STOP network, which already provides the housing services, would provide the additional services as well. Absent the proposal, funding for the program would expire June 30, 2024.
Assessment
Inflation Increases Appear Reasonable for Parole Rehabilitation Programs
Cost‑of‑living increases for parole rehabilitation programs appear reasonable because it could mitigate the erosion of the quantity and quality of services that can be caused by inflation. Because costs have increased due to inflation in recent years, it is plausible that providers are less willing to extend their existing contracts. In addition, other providers that don’t already offer these services (1) may be less willing to do so, (2) would do so by providing lower‑quality services, or (3) would provide services to fewer people. This trend would make it difficult for CDCR to find quality providers and ensure people on parole receive rehabilitation programming. For example, CDCR reports it was not successful in obtaining bids for DRC and LTORR contracts that had been set to expire at the end of 2023‑24, which were advertised at the same or similar rates to the prior contracts for these services. The department reported that the 2024‑25 funding increases for those contracts appear to have allowed it to successfully obtain contractors for some of these services, though the contracting process is still ongoing.
Parole Rehabilitation Programs Have Not Been Evaluated for Cost‑Effectiveness
Ensuring that programs are cost‑effective helps ensure that the state is allocating its limited resources for rehabilitation programs in a manner that has the maximum effect on people successfully completing their parole terms and not committing additional crime. Accordingly, to the extent that the state is not allocating its resources to the most cost‑effective programs, it is potentially allowing more crime to occur than would otherwise be the case. Although some metrics exist about participants, the department generally lacks robust evaluations of the actual cost‑effectiveness of its parole rehabilitation programs. This makes it difficult for the department to determine which rehabilitation programs are cost‑effective, whether there are potential obstacles or challenges preventing them from operating cost‑effectively, and whether some are more cost‑effective than others. As such, it is difficult for the Legislature to assess which programs are the most successful at reducing recidivism and to target funding towards those programs.
Current Structure of STOP Makes It Costlier to State and Potentially Less Effective
Medi‑Cal SUD Treatment Has Advantages Over CDCR’s SUD Treatment for People on Parole. In our publication Improving Parolee Substance Use Disorder Treatment Through Medi‑Cal, we found that SUD treatment provided through Medi‑Cal has several advantages over CDCR‑funded SUD treatment. Specifically, Medi‑Cal‑funded SUD treatment (1) provides care based on medical necessity, (2) allows care to continue beyond parole, and (3) makes greater utilization of federal funding—all of which the existing parole SUD treatment structure under STOP does not do. In addition, nearly all Medi‑Cal enrollees in the state receive comprehensive SUD treatment services modeled after the American Society for Addiction Medicine Criteria. These findings indicate that the state is operating a parole SUD treatment system that is potentially less effective and costlier than Medi‑Cal’s existing SUD treatment structure.
STOP Report Suggests Many CDCR‑Funded Providers Either Already Are Medi‑Cal Licensed Providers or Are Interested in Becoming So. In December 2024, CDCR surveyed over 80 STOP network providers on the feasibility of becoming Medi‑Cal licensed providers. This would be necessary for these providers to give Medi‑Cal funded care to people on parole. Over half of the respondents indicated that they are in the process or would like to become Medi‑Cal licensed providers. The survey findings are encouraging in that they indicate a willingness from providers to leverage Medi‑Cal SUD treatment. To the extent these providers are able to become Medi‑Cal licensed providers and CDCR is able to successfully refer people on parole to them, it could improve the quality of care and reduce state costs. The CDCR report did, however, outline challenges STOP network providers cited in transitioning to Medi‑Cal. For example, some providers indicated they had not pursued Medi‑Cal licensure due to not knowing how to apply, administrative burdens, and cumbersome certification requirements. The report also suggests that some of these challenges could be addressed through technical assistance.
Ongoing Need for RHW Unclear
Lack of RHW Report Makes It Difficult to Assess Effectiveness of Program. Because the report on the metrics and outcomes associated with RHW will not be available until March of 2026, it is difficult for the Legislature to assess whether the program merits ongoing funding. For example, the department is expected to report on return‑to‑prison rates, reconviction rates, and housing status after leaving the program for RHW participants. Without such information, it is difficult to know whether the program is effective at reducing crime or homelessness among those exiting prison.
Under CalAIM, Medi‑Cal Could Provide Similar Services as RHW, Potentially at a Lower State Cost. As discussed above, under CalAIM, Medi‑Cal managed care plans are starting to provide housing services targeted to those at risk of homelessness and those transitioning from incarceration, which would include people on parole. This means the program targets a very similar population as RHW. For example, under CalAIM, Medi‑Cal already provides housing services—such as housing deposit support—to high‑risk, high‑need populations. Moreover, Medi‑Cal managed care plans will eventually be required to provide access to six‑month transitional housing rental assistance to eligible populations, including people on parole. To the extent people on parole receive these services, the state could draw down federal funds for those that are Medi‑Cal eligible, potentially resulting in lower state costs than providing these services through RHW.
Recommendation
Require CDCR to Increase Utilization of Medi‑Cal for Parole SUD Treatment and Require Evaluation
Require CDCR to Increase Utilization of Medi‑Cal for Parole SUD Treatment. In order to capitalize on the advantages of Medi‑Cal‑funded SUD treatment programs for people on parole and the willingness of some providers to become Medi‑Cal licensed providers, we recommend a series of steps to increase the utilization of these programs for people on parole. These steps are outlined in detail in our report Improving Parolee Substance Use Disorder Treatment Through Medi‑Cal. Below, we provide a summary of these steps, which would improve the quality of parole SUD treatment while allowing the state to draw down additional federal funding in place of state funding.
- Connect All People on Parole With Medically Appropriate SUD Treatment. We recommend the Legislature require CDCR to refer all people on parole with a medical need for SUD treatment to Medi‑Cal licensed providers in the community. This process should be facilitated by the fact that CDCR already screens people for medical SUD treatment needs and helps people submit Medi‑Cal applications while they are in prison.
- Require STOP Network Providers Become Medi‑Cal Providers and Ensure Continuity of Care. We recommend that the Legislature direct CDCR to require all STOP network providers to become Medi‑Cal licensed providers and require that STOP network providers continue services after people are discharged from parole. This would help ensure that people on parole receive medically appropriate SUD treatment based on their needs during and after parole.
- Structure Funding to Streamline Billing and Reduce Workload. We recommend requiring STOP network providers to submit their expenditures for reimbursement using the existing Medi‑Cal billing structure. This would eliminate the need for funding for services provided to people on parole to pass through the regional STOP contractors. Instead, this process would require that STOP network providers submit their expenditures for reimbursement to counties who would then submit their expenditures to DHCS for either state or federal reimbursement. This approach would also prevent STOP network providers from needing to bill both CDCR and counties.
- Ensure Costs Are Not Shifted to Counties and Nonreimbursable Services Maintained. Under our recommendations above, there could be costs shifted to counties—especially for STOP services that are not covered through Medi‑Cal and portions of costs that the federal government does not pay. To ensure such costs are not shifted to counties and nonreimbursable STOP services are maintained, the Legislature could direct DHCS to pass those costs to CDCR.
Under this structure, most expenditures on parole SUD treatment would shift from CDCR to Medi‑Cal. As such, CDCR would eventually no longer need the full $98 million (General Fund) currently proposed for STOP in 2025‑26, which includes the $28.3 million cost‑of‑living increase requested for these services. While this would increase Medi‑Cal costs, it would allow for federal reimbursements for a significant portion of the cost of parole SUD treatment service. We estimate this could generate low to mid tens of millions of dollars in net General savings annually.
Provide Requested STOP Funding on a Limited‑Term Basis to Allow for Transition. We acknowledge that it would take time to implement our recommendations highlighted above. As a result, we recommend funding the portion of the Governor’s proposal related to STOP ($28.3 million) for at least one year. This would provide CDCR, DHCS, counties, and the STOP network providers time to implement our recommendations.
Direct CDCR to Contract for Evaluation of Restructured Parole SUD Treatment Programs. As discussed above, parole rehabilitation programs—including parole SUD treatment—have not been evaluated for cost‑effectiveness, making it is difficult to know whether the programs are achieving the goals at the lowest possible cost. To address this, we recommend that the Legislature direct the department to partner with external researchers to evaluate parole SUD treatment following the changes discussed above. This could result in some modest additional one‑time costs for the department that would likely be far outweighed by the savings that would be achieved from increasing the use of Medi‑Cal for parole SUD treatment.
Reevaluate Ongoing Need For RHW Proposal
Consider Approving Funding on One‑Year Basis. To the extent RHW remains a legislative priority, we recommend the Legislature modify the proposal by funding it on a one‑year basis instead of two. In March 2026, the Legislature expects to receive more information about RHW implementation, including preliminary rates at which people in the program recommit crimes. With this information, the Legislature will be in a better position to revisit the RHW funding level as it deliberates on the 2026‑27 budget.
Modify RHW Reporting Requirement to Require Assessment of Using Medi‑Cal for Housing Services. In light of the availability of housing assistance programs under CalAIM, we recommend that Legislature modify the RHW reporting requirement to mandate that CDCR (in consultation with DHCS) also include an analysis of the viability of relying on Medi‑Cal rather than RHW for housing people on parole. Under this approach, CDCR would connect people on parole to Medi‑Cal providers in the community that can help them receive housing services rather than using RHW. In the report, CDCR should, at minimum, provide information on the relative state cost of relying on Medi‑Cal versus RHW and what the pros and cons of RHW and Medi‑Cal funded services are. This would allow the Legislature to assess whether RHW merits separate ongoing funding or if CDCR can instead rely Medi‑Cal to provide housing services to people on parole at a lower state cost.
Fund Remaining Programs on a Limited‑Term Basis and Require Evaluation
Require Evaluation of DRC and LTORR. Given that DRCs and LTORR programs have not been evaluated for cost‑effectiveness, we recommend that the Legislature direct CDCR to partner with external researchers to do so. Such an evaluation could result in modest one‑time costs to CDCR that would likely be absorbable, though the Legislature could work with the department to determine whether dedicated funding is necessary. We think that the modest costs to the state would be justified, as the evaluation would allow the Legislature to determine whether these programs—totaling over roughly $40 million in annual spending—merit continued support or need to be restructured to be effective. We recommend this evaluation be provided to the Legislature no later than January 10, 2029 to provide the external evaluator time to complete the review.
Provide Funding on Limited‑Term Basis Pending Results of Evaluation. To maintain these programs in operation while the evaluation is being carried out, we recommend providing three years of the proposed increases in funding for DRCs and LTORR programs ($3.7 million in 2025‑26, $4 million in 2026‑27, and $4.4 million in 2028‑29). This would allow the Legislature to review the evaluation as part of its deliberations during the 2029‑30 budget process, at which point it could consider whether to provide ongoing funding for these DRCs and LTORR programs.
Air Cooling Pilot Program
Background
Many Prisons Experience High Summer Temperatures and Lack Adequate Cooling. Many of the state’s prisons are located in areas that experience high summer temperatures, including the eastern and southeastern deserts, Central Valley, Antelope Valley, and Inland Empire. CDCR has traditionally used evaporative cooling (a system that cools air through evaporation of water, sometimes called a “swamp cooler”) for the majority of housing areas. These systems were designed to keep indoor temperatures under 89 degrees Fahrenheit, though the department reports that its existing systems are not always capable of meeting even this standard.
High Heat Poses Health and Other Risks for People Who Live and Work in Prisons. In hotter temperatures, the body must work harder to cool itself. When the body’s temperature control system cannot do so, significant physiological problems can occur—such as fainting, nausea, muscle cramps, damage to vital organs, and in extreme cases, death. These problems can set in more quickly for people who take medications (such as diuretics, antihistamines, and many mental health medications) or have other health conditions (such as cardiovascular disease or diabetes) that impair their body’s temperature control system. Risk of heat‑related illnesses also increases as humidity rises. Moreover, use of portable electric fans in certain hot conditions can speed the onset of heat‑related illnesses by blowing hot air on the body and increasing the heat stress that the body must respond to. In addition to its direct risks to health, heat may also limit productivity (such as in education classes) and some studies indicate it is correlated with violence and self‑harm.
CDCR Has Various Heat‑Related Policies. CDCR has various policies intended to mitigate some of the negative effects of heat. For example, when indoor temperatures reach 90 degrees, staff initiate cooling and hydration procedures such as cool showers and misting and perform increased observation of people with health conditions that make them particularly sensitive to heat.
CDCR Is Likely to Face Requirements to Limit Indoor Heat in Prisons. In July 2024, the Occupational Safety and Health Standards Board (OSHSB) approved a regulation requiring employers to take steps to protect workers from heat when indoor temperatures reach 82 degrees Fahrenheit, with additional requirements when temperatures reach 87 degrees Fahrenheit. Local and state correctional facilities were exempted from these regulations. However, OSHSB is in the process of developing an industry‑specific regulation for workers in local and state correctional facilities. In addition, plaintiffs in an ongoing class action lawsuit related to prison medical care (known as Plata v. Newsom) have expressed concerns about extreme heat, suggesting that heat‑related litigation is possible.
Governor’s Proposal
Install and Evaluate Three Options for Cooling in Four Types of Housing Units. The Governor proposes $23.6 million in 2025‑26 and $45.4 million in 2026‑27 from the General Fund for a pilot program to install and evaluate three options to reduce indoor temperature in certain housing units at the Central California Women’s Facility in Chowchilla; California Medical Facility in Vacaville; Kern Valley State Prison in Delano; and California State Prison, Los Angeles County in Lancaster. Specifically, the pilot would test: (1) mechanical cooling (such as air conditioning) only, (2) exterior thermal insulation only, and (3) mechanical cooling plus thermal insulation. These options would be installed in four different housing unit design types that are common throughout the prison system. The department reports that it identified the cooling options through an engineering study of the existing infrastructure in these four housing unit types and what modifications would be capable of maintaining interior temperatures below 79 degrees Fahrenheit. Based on this study, the department is expecting mechanical cooling and mechanical cooling plus insulation to meet this temperature goal. It expects thermal insulation alone to provide temperature reductions but acknowledges that it is not expected to meet the 79 degree threshold. However, because insulation is relatively quicker and less expensive to install than mechanical cooling, the department considers it worth piloting. CDCR expects installation for the pilot to be completed in 2028‑29 and intends to use the findings to inform a plan to cool facilities statewide.
Assessment
Piloting Cooling Options Makes Sense. In view of the health and other risks posed by indoor heat as well as the likelihood that the state will face requirements related to indoor heat in prisons, it makes sense to proactively begin addressing the issue. In addition, piloting alternatives in four common housing unit design types is a reasonable step to inform a broader statewide strategy.
Department Has Not Provided a Detailed Plan to Evaluate Success. The department has not provided a detailed plan for how it would evaluate success in the pilot. For example, it has not described its plan for measuring temperature, such as whether it would use sensors located throughout housing units that continuously measure and transmit data or whether it would depend on staff to manually read and log temperatures. The department has also not specified the data to which it will compare the pilot sites. For example, it is unclear if it would compare pilot housing units to their own interior temperatures from previous years or if it would compare pilot housing units to data collected from other housing units over the same time period.
Systemwide Implementation Could Present Significant Challenges. While the exact scope of the problem is not clear, it seems likely that meeting the 79 degree goal statewide could be a major undertaking. Specifically, we find that statewide implementation could present the following significant challenges:
- High Cost. The department has not developed a cost estimate or time line to scale up air cooling because it intends to use the results of the pilot to inform its statewide strategy. However, our rough estimates suggest that the one‑time installation costs to cool facilities statewide could total in the low billions of dollars. In addition, operation of mechanical cooling systems would increase ongoing utility costs. The department’s engineering study estimates that the addition of mechanical cooling for facilities that previously have only included evaporative cooling will increase annual energy costs by $77,000 to $141,000 annually per building. If scaled up statewide, we estimate that the increase in CDCR’s energy costs could be in the tens of millions of dollars annually.
- Additional Strain on Project Planning and Management Capacity. The potentially high cost of installing air cooling statewide would be in addition to the roughly $1.5 billion in other infrastructure projects that CDCR estimates it will need to pursue over the next decade to address issues related to safety (such as replacement of fire suppression systems) and critical infrastructure (such as kitchen renovations). Accordingly, introduction of air cooling projects alone could potentially double the volume of projects over this time period. This would put additional strain on CDCR’s project planning and management capacity, which is concerning given that effective project planning and management is important for ensuring projects are completed in an efficient and timely manner.
- Operational Considerations Could Limit Implementation Speed. CDCR indicates that installation of mechanical cooling could cause operational disruptions to housing units during construction, though the details cannot be determined until design is complete. To the extent people need to be relocated to other housing units during construction, this would limit the number of projects that can be ongoing at any given time. This is because the more housing units that are under construction at a given time, the more people will become concentrated in the remaining housing units. Accordingly, to avoid overcrowding, the department would likely have to pursue statewide implementation in several construction stages, which could take many years to complete.
Legislature Needs Additional Information to Provide Ongoing Oversight. Given the serious health risks posed by extreme heat in prisons and the significant challenges that could come with systemwide implementation of air cooling, it is important that the Legislature has information necessary to provide oversight going forward. For example, it might make more sense to close, or even rebuild, a prison with particularly significant infrastructure problems rather than pay to repair and upgrade it. However, to make this decision, the Legislature would need information about the condition of the infrastructure and estimated costs and time lines to address it. In addition, the Legislature needs information about what other strategies—besides major infrastructure modifications—CDCR is considering to mitigate heat. This is important because the pilot will not be completed until 2028‑29 and statewide implementation could take many years more. Accordingly, interim strategies to address heat are essential to mitigating health and litigation risks in the near term.
Recommendation
Approve Pilot. Given the health risks of extreme heat, the risks of heat‑related litigation, and the reasonable approach to testing various air cooling alternatives proposed by the Governor, we recommend approving the proposed air cooling pilot.
Require CDCR to Provide Evaluation and Statewide Strategy by January 10, 2031. We recommend that the Legislature adopt trailer bill language requiring CDCR to provide an evaluation of the pilot by January 10, 2031 (a full year and a few months after the installation of the air cooling projects at the pilot sites is expected to be completed). To inform this trailer bill, we also recommend directing CDCR to provide during spring 2025 budget hearings a clear plan for how it will evaluate success in the proposed pilot. In addition to the evaluation, the department should submit in the January 10, 2031 report a recommended statewide strategy for scaling air cooling in a timely and efficient manner. To the extent the strategy would involve deactivating housing units while air cooling is being installed, the report should discuss how CDCR would manage the impact to the prison population and employees. In addition, the report should include consideration of options to expedite construction.
Require CDCR to Provide an Interim Report by January 10, 2026 With Information Necessary for Legislative Oversight. We recommend that the Legislature adopt budget bill language requiring CDCR to report by January 10, 2026 on the following:
- Systemwide Monitoring. The report should discuss the administration’s current capabilities and/or plans to collect statewide data on temperature, humidity, and the availability of electric fans in housing units as well as other areas of prisons that may also require cooling, such as kitchens. Such data would be useful for CDCR and the Legislature in determining how to prioritize deployment of future cooling interventions. For example, if fans are not authorized in certain units due to security reasons or physical plant limitations, it could make sense to prioritize these units to receive mechanical cooling.
- Status of Existing Infrastructure. For each housing unit in the state, the report should indicate (1) their design type, (2) their existing air cooling infrastructure (if any), and (3) how many days they exceeded 78 degrees over the past year (or similar available data).
- Plan for Nontypical Housing Units. For those housing units that are not one of the four common design types included in the pilot, the report should discuss the steps CDCR has taken and/or plans to take (such as conducting additional engineering studies) to identify cooling options for them.
- Other Heat Mitigation Strategies. The report should discuss other policies and/or practices CDCR has adopted or is considering to mitigate the effects of indoor heat in the near term. For example, these may include using portable air conditioning units, changing lightbulbs to LED, reducing humidity (such as by ensuring showers are properly ventilated), painting roofs to reflect solar radiation, modifying summer uniforms, creating cooling centers, or changes to policies for monitoring and responding to heat‑related illnesses. In particular, the report should include a discussion of policies around electric fan usage, given that they can be helpful in some circumstances but increase risk of heat‑related illness in others.
Appendix
Appendix Figure 1
Summary of LAO Recommendations
|
Issue |
Governor’s Proposal |
LAO Recommendation |
|
State Prison and Parole Population and Other Biannual Adjustments |
The budget estimates that Proposition 36 (2024), which increased punishment for various theft and drug crimes, will cause the average daily prison population to be about 570 higher (1 percent) than otherwise in 2024‑25 and 3,300 higher (4 percent) in 2025‑26. It estimates that Proposition 36 will not impact the average daily parole population in 2024‑25 but will cause the population to be about 360 higher (or 1 percent) than otherwise in 2025‑26. |
Direct the California Department of Corrections and Rehabilitation (CDCR) to address certain flaws in its estimates, which likely cause it to be over budgeted by millions of dollars in 2024‑25 and tens of millions of dollars in 2025‑26, and adjust its funding requests at the May Revision accordingly. |
|
San Quentin Rehabilitation Center (SQRC) and the California Model |
$7.8 million in 2025‑26 (growing to $13 million by 2027‑28) from the General Fund for SQRC to activate a new learning center and make other programmatic enhancements (such as establishing a new bachelor’s degree program). The proposal is part of a systemwide effort to develop the “California Model,” which is broadly intended to reduce recidivism and improve the health and wellness of people who live and work in prison. |
While it is reasonable to activate the new learning center, most of the remainder of the request is premature and we recommend rejecting it unless the administration is able to provide a clear plan for SQRC. In addition, we recommend requiring the administration to produce a report that answers a variety of key questions that remain unanswered about the California Model. |
|
Inpatient Mental Health Beds |
$3 million General Fund in 2025‑26 (growing to $4.4 million in 2026‑27 and ongoing) to activate a newly constructed, licensed, 50‑bed mental health crisis facility at the California Institution for Men in Chino. |
Approve activation of the facility. Direct CDCR to seek approval from the Coleman federal court to align inpatient bed capacity with updated population projections and to account for transportation savings. These changes could reduce CDCR costs by more than $100 million annually if all the excess beds are deactivated. |
|
Suicide Watch |
$13.6 million General Fund in 2025‑26 and ongoing for suicide watch workload. |
Approve one‑time funding. Direct CDCR to take the following steps to reduce costs of suicide watch: (1) continue efforts to fill Certified Nursing Assistant suicide watch vacancies, (2) create an alternative classification for this work, and (3) direct CDCR to develop a population‑driven budgeting methodology. |
|
Parole Community Rehabilitation Programs |
$44.9 million General Fund in 2025‑26 (generally increasing annually thereafter) for various parole rehabilitation programs. |
Approve the proposed funding on a limited‑term basis and require CDCR to take steps to increase utilization of Medi‑Cal for some of these programs, which could improve them while reducing state costs. Direct CDCR to evaluate all of these programs to determine whether they merit continued support or need to be restructured to be effective. |
|
Air Cooling Pilot Program |
$23.6 million in 2025‑26 and $45.4 million in 2026‑27 from the General Fund for a pilot program to install and evaluate three options to reduce indoor temperature in prisons. |
Approve proposal, but adopt legislation requiring an evaluation and statewide strategy to expand air cooling by January 10, 2031 and an interim report with information necessary for legislative oversight of CDCR’s air cooling efforts by January 10, 2026. |
