LAO Contact
Other Reports in This Series
April 5, 2022
Climate Change Impacts Across California
Health
- Summary
- Introduction
- Major Climate Change Impacts On Health
- Significant Existing Efforts and Funding
- Key Issues for Legislative Consideration
- Conclusion
Summary
Climate change will have a number of serious impacts on California, including public health risks, damage to property and infrastructure, life‑threatening events, and impaired natural resources. This report focuses on how a changing climate is affecting the health of Californians and key issues the Legislature faces in responding to those impacts. This is one of a series of reports summarizing how climate change will impact different sectors across California.
We find that climate change has a wide variety of direct and indirect health effects on Californians. In particular, rising temperatures and extreme heat events are projected to increase deaths and exacerbate conditions like cardiovascular disease and kidney failure. Similarly, additional wildfire smoke driven by a changing climate leads to higher levels of respiratory illness, preterm births, and deaths. The adverse health effects are not uniformly distributed across regions and populations, however. Some areas are more susceptible to climate‑induced disasters or other changes, or are less able to adapt to these changing conditions. Certain populations, particularly lower‑income, older, or medically compromised individuals, as well as outdoor workers, will disproportionately bear the adverse health burdens of climate change. Finally, changing climate conditions likely will challenge the state’s health care delivery system in multiple ways—including placing additional strain on emergency response systems and increasing demand for climate‑related services—although the magnitude of these challenges is not yet well known.
As the Legislature considers various climate adaptation strategies within the health policy domain, it will first want to consider how state health policies and programs fit into the broader set of actions taken by individuals, the private sector, local governments, and other state agencies. For example, state health departments can play a vital role in supporting research on the health effects of climate change; improving data collection, sharing, monitoring, and analysis; and evaluating which health‑related climate adaptation activities are most effective and efficient. This information can be used to assist and support other state agencies and local governments. The Legislature also may want to consider ways to ensure health care delivery systems are adequately prepared to respond to climate change, particularly climate‑induced disasters. Finally, the Legislature will want to think about how the state can reduce adverse health impacts on the most vulnerable populations. For example, state policies and funding could be targeted in ways that support populations lacking the resources to adequately protect themselves from the increasing health risks.
Introduction
This report contains three primary sections: (1) the major ways climate change affects health, (2) significant existing state‑level efforts underway to address climate change impacts in the health sector, and (3) key questions for the Legislature to consider in response to these impacts. Given the complexity of the issues, this report does not contain explicit recommendations or a specific path forward; rather, it is intended as a framing document to help the Legislature adopt a “climate lens” across the health policy area.
Because some degree of climate change already is occurring and more changes are inevitable, this document focuses primarily on how the Legislature can think about responding to resulting impacts. Of note, the state is also engaged in numerous efforts to limit the degree to which climate change occurs by enacting policies and programs to reduce emissions of greenhouse gases (GHGs).
California Faces Five Major Climate Hazards. As discussed in depth in our companion report, Climate Change Impacts Across California: Crosscutting Issues, California faces five major hazards as the result of climate change. Specifically, increasing temperatures, a changing hydrology, and rising sea levels will lead to:
- Higher average temperatures and periods of extreme heat.
- More frequent and intense droughts.
- Increased risk of floods.
- More severe wildfires.
- Coastal flooding and erosion.
Below, we discuss specific impacts these hazards will have on health.
Major Climate Change Impacts On Health
While climate change will have myriad and increasingly adverse health effects on Californians, thus far, rising temperatures, extreme heat events, and wildfire smoke are creating some of the worst problems, including exacerbating cardiovascular disease and respiratory illnesses. Below, we discuss (1) many of the key types of health risks associated with climate change, (2) some of the available research about the magnitude of some of the major effects, (3) how these impacts are disproportionately spread across regions and populations, and (4) how climate change could affect health care delivery systems.
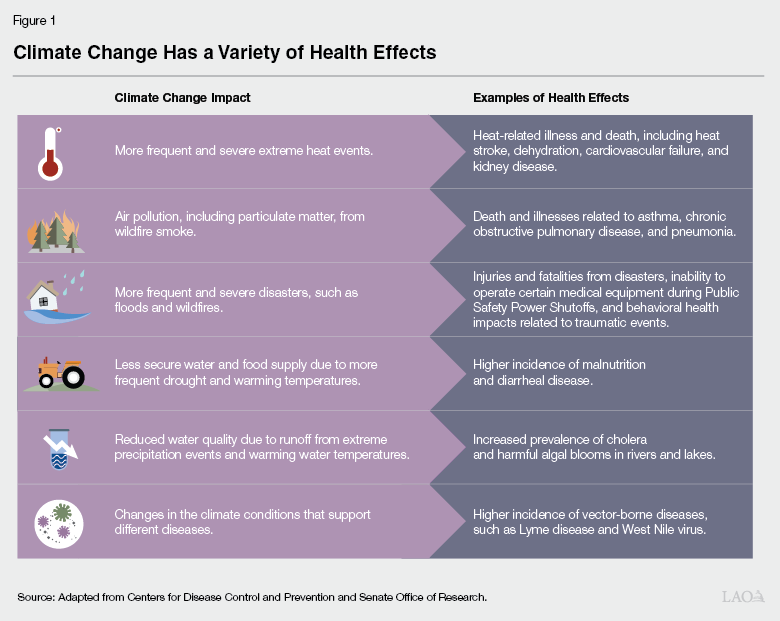
Climate Change Has a Wide Variety of Health Effects. As shown in Figure 1, climate change has a wide variety of human health effects. Some of the most direct impacts include injuries, illnesses, and deaths related to extreme heat; disaster events (such as floods and wildfires); air pollution; changes in water quality; impacts on food and water supplies; and increasing prevalence of certain diseases. In addition, there are other indirect avenues through which climate change affects human health. For example, some studies have found that higher temperatures can reduce worker productivity and student learning. Since there is often a link between economic outcomes (such as income) and human health, adverse effects on economic outcomes caused by climate change (such as reduced wages or gross domestic product) can affect human health indirectly.
Extreme Heat Is Likely One of the Most Significant Factors Impacting Mortality in California. Temperature‑related mortality (including from extreme heat) is projected to be among the most deadly and costly impacts of climate change in certain locations around the globe. Higher temperatures and extreme heat can lead to heat stroke and increase the risk of or exacerbate cardiovascular disease, respiratory disease, kidney failure, and preterm births. Extreme heat is already one of the top contributors to weather‑related deaths in the United States and California. For example, data from the California Department of Public Health (CDPH) show that from 2010 through 2019, California experienced roughly 600 deaths for which heat was the primary cause of death, and other analyses that attempt to measure impacts on overall mortality estimate an additional 3,300 deaths for which heat was a contributing factor. The number of heat health events (HHEs)—defined as a set of temperature and humidity conditions over a period of several days that are known to result in significant negative health effects—are projected to grow in California in the coming decades. Under a moderate‑emissions scenario—which assumes that international practices result in the rate of worldwide GHG emissions slowly declining in the coming decades, somewhat constraining the magnitude of global temperature increases—annual net mortality effects related to increased temperatures are projected to be 9 deaths per 100,000 people in California. (While the U.S. average is close to zero, projections vary state by state.) By comparison, the 2019 annual mortality rate from automobile accidents in California was about 9 deaths per 100,000 people and from drug overdose about 15 deaths per 100,000 people. As discussed in more detail below, adverse health effects of hotter temperatures will be particularly significant in some locations and for certain populations.
New Research Suggests Adverse Health Effects From Wildfire Smoke Also Are Substantial. Poor air quality has been linked to a wide variety of adverse health effects, including increased risk of asthma, cardiovascular disease, cognitive impairment, and premature births. California already has some of the most significant air quality challenges in the country, largely related to human activities (such as driving gasoline‑ and diesel‑powered vehicles) and the geography of certain regions that trap air pollutants. For example, the San Joaquin Valley and South Coast air basins have some of the worst air pollution in the nation. In recent years, smoke from wildfires has grown substantially and has been a major contributor to air pollution in the western United States—making up roughly half of small particulate matter in some regions, compared to less than 20 percent a decade ago. Overall health effects from wildfire smoke are still being studied, but a rough estimate suggests wildfire smoke in 2020 caused about 20 deaths per 100,000 adults over the age of 65. Wildfire smoke also can have long‑term health effects. For example, it has been linked to an increase in preterm births, which in turn increases the risk of various long‑term health problems for those children. The degree to which climate change will impact particulate matter emissions in the future is subject to some uncertainty, but one study of California wildfires estimates that particulate matter in fire‑prone areas could roughly double by the end of the century. Another recent study by Stanford University researchers estimates that a 50 percent increase in wildfire smoke could increase deaths of older adults by an additional 9 to 20 per 100,000 people annually, an impact that is similar to the projected temperature‑related mortality discussed earlier.
Type and Magnitude of Impacts Vary Substantially by Region and Community. The type of climate impacts and the magnitude of those effects will vary by location. For example, the projected number of HHEs will differ significantly across different regions of the state. Under a high‑emissions climate scenario where annual GHG emissions grow substantially over the next several decades, some regions—such as parts of Riverside and Placer Counties—are expected to experience five additional HHEs annually by mid‑century, compared to fewer than one additional HHE annually in other regions such as many coastal areas and large areas of Northern California. Notably, even though extreme heat will be more frequent and severe in hotter regions, one national study by researchers from the National Bureau of Economic Research estimates that temperature‑related mortality is actually projected to be higher in cooler regions because they are less prepared for the heat (for example, fewer buildings have air conditioning). There also are significant differences in the projected number of heat‑related deaths within a particular region or city. For example, urban areas with a large percentage of impervious surfaces and relatively little shade—also known as urban heat islands—tend to be hotter than surrounding areas. These urban heat island effects tend to be more severe in neighborhoods that were the subject of historical discriminatory housing policies, such as redlining.
Similarly, the effects of wildfire on health will vary across regions. The direct impacts—such as deaths and injuries occurring in and adjacent to the fires—will be concentrated in areas where people live near fire‑prone landscapes, typically in rural areas or in the wildland‑urban interface. While communities near fire‑prone areas also will experience more significant impacts from wildfire smoke and loss of power during Public Safety Power Shutoff (PSPS) events, these indirect effects also can impact other regions of the state (as well as other states). For example, effects can be more widespread when wind transports wildfire smoke to other parts of the state and if utilities shut down a major electricity transmission line during a PSPS event.
Vulnerable Populations Will Bear a Disproportionate Burden of Impacts. Within a particular region or community, some populations will be more impacted by climate change than others. In general, low‑income households and communities are expected to bear a disproportionate burden because they have fewer resources to adapt to various climate impacts. For example, low‑income households have less money to purchase and operate air conditioning units during extreme heat events, air filters to moderate wildfire smoke, or back‑up electricity generators to provide electricity during PSPS events. In addition, some of the most significant climate impacts—such as heat and wildfire smoke—disproportionately affect certain medically vulnerable populations, including children and the elderly, populations that have underlying medical conditions (such as asthma and cardiovascular disease), and populations that spend a lot of time outdoors (such as homeless populations and outdoor workers). Extreme heat and wildfire smoke that make it dangerous to spend time outside during certain times also could disproportionately affect people who are institutionalized (such as patients at State Hospitals and individuals in state prisons and county jails). These populations might not have an opportunity to go outside for days at a time because they are only allowed to spend time outside during specific hours of the day.
Climate Impacts Will Have a Wide Variety of Effects on Health Care Delivery Systems. Changing conditions and more frequent emergency events will challenge health care delivery systems in multiple ways, including:
- Additional Strain on Emergency Operations. Climate change can strain health care professionals and facilities needed to treat patients during more frequent and severe emergencies. When facilities, workers, and transportation and power systems themselves are affected by the emergency (for example, if a hospital and its workers must evacuate during a wildfire), capacity in nearby areas and the ability to deliver timely care could be impaired. Following the 2018 Camp Fire, for example, nearby health systems in Butte County experienced increased demand due to the loss of 100 staffed hospital beds in Paradise.
- Increased Demand for Certain Services. A changing climate also could increase ongoing demand for services to treat certain conditions that are exacerbated by climate change, such as heat‑related illnesses, respiratory diseases, and behavioral health needs related to trauma and anxiety. This could amplify the need for professionals trained to treat these increasingly common conditions.
- Greater Need for Information Sharing. Currently, only limited data sharing occurs among health plans, public agencies, providers, and facilities, making planning for emergencies and treating patients during disasters more difficult. As noted below, the state has developed a system for emergency responders to access some patient health information during an emergency—the California Patient Unified Lookup System for Emergencies (PULSE)—but it has limited functionality. A more systematic exchange of information would aid state and regional planning for health care workforce, equipment, and supply needs. Increased data sharing also would facilitate better real‑time notification across provider systems about disease spread or anticipated health threats from disaster events. Moreover, when a patient has to be transported from one facility to another during an emergency, reliable access to the patient record is vital to ensuring continuity of care.
- Reduced Availability of Workforce and Care. Similar to many other industries, climate change could affect the supply of health care workers and facilities in particular areas. For example, in the short term, the availability of health care workers is impacted when a disaster damages their homes or the facilities at which they work or leads to an evacuation order. In the long run, providers might choose to work elsewhere due to climate change risks. Given the essential role of health care systems, particularly in emergency situations, even short‑term shortages could complicate the state’s long‑term planning efforts to ensure there are sufficient providers in all areas of the state.
The overall magnitude of these different effects on health care delivery systems in the coming decades still is unclear.
Significant Existing Efforts and Funding
The state already has undertaken some steps to begin addressing how the changing climate impacts Californians’ health. Some of these activities have been in direct response to climate change, while others—such as those that seek to address the social determinants of health or to improve responses to emergencies—have complementary primary goals that also have climate‑related benefits. Below, we highlight some of these recent efforts.
CDPH Climate Change and Health Equity Section. Within CDPH’s Office of Health Equity (OHE), the Climate Change and Health Equity Section consults and collaborates with other state and local agencies to ensure social determinants of health are addressed in their climate adaptation activities. Activities include providing technical assistance, data, research, toolkits, and interactive web resources.
CALBRACE Tool. California is one of 16 states and 2 cities receiving special Centers for Disease Control and Prevention funding to plan for the health impacts of climate change. California’s program, California Building Resilience Against Climate Effects (CalBRACE), housed in CDPH’s OHE, is focused on the health impacts of rising temperatures and extreme heat, wildfire, and sea‑level rise. CalBRACE provides tools to local governments to aid in their planning efforts, such as county‑level profiles on climate change and health, and data visualizations on health vulnerabilities.
Medi‑Cal Reforms to Address Social Determinants of Health. The recently approved California Advancing and Improving Medi‑Cal (CalAIM) reform effort seeks to improve the health of Medi‑Cal’s highest‑need beneficiaries by addressing the social determinants of health, which also helps these individuals adapt to the health impacts of climate change. For example, under CalAIM, Medi‑Cal plans have the option to pay for air conditioners and asthma remediation services.
Ensuring Access to Health Care During and After States of Emergency. State law requires health plans to ensure continued access to medically necessary health care services for enrollees affected by a state of emergency and allows them certain flexibilities (such as suspending prescription refill limitations). Existing state and federal Medicaid laws also allow the waiver of Medi‑Cal program rules during and after emergencies. For example, providers may receive reimbursement for services delivered via telehealth and the state may presume Medi‑Cal eligibility for likely eligible applicants.
Development of New Data Exchange Framework. Chapter 143 of 2021 (AB 133, Committee on Health) requires that the California Health and Human Services Agency create a data exchange framework to facilitate sharing of health and social services information across health care entities (health plans, providers, facilities, and labs) and government agencies over the next several years. While not specifically proposed in response to climate change, this effort will enable sharing of additional real‑time health information during climate‑driven emergencies.
Augmentations to Emergency Medical Services Authority (EMSA) Budget. EMSA develops and implements emergency medical services and aids in preparing for, coordinating, and supporting state and local emergency medical response to disaster events. The 2021‑22 state budget augmented EMSA’s funding by $36 million one‑time across three years and $3.3 million ongoing to increase the authority’s capacity, including for medical surge staffing, storage and maintenance of emergency equipment and supplies, regional disaster medical health response, and planning for development of a statewide emergency services data resources system.
Access to Patient Health Care Information During Emergencies. EMSA manages the PULSE system, which provides specified health care workers who are volunteering during an emergency short‑term access to patients’ personal health information. The system has been activated during recent years’ wildfires.
Climate Adaptation Funding Included in 2021‑22 Budget. The most recent state budget included various multiyear funding packages that are meant to promote climate adaptation, including $3.7 billion for climate resilience activities (including for extreme heat), $4.6 billion for drought and water resilience activities, and $988 million to address wildfire and forest resilience. The funds will be administered primarily by natural resources and environmental protection departments but will support activities that could reduce negative health impacts.
Key Issues for Legislative Consideration
The Legislature has a wide range of potential state policy and budget actions it could undertake to reduce the adverse effects of climate change on health. Below, we raise several questions the Legislature will want to consider as it thinks about the role of health policies, programs, and delivery systems in adapting to the impacts associated with a changing climate. We also summarize these issues in Figure 2.
Figure 2
Climate Change Impacts on Health:
Key Issues for Legislative Consideration
|
|
|
|
|
|
|
How Should State Health Policies and Programs Fit Within the Broader Suite of Adaptation Activities? The magnitude and extent of climate change impacts on the health of Californians makes it unreasonable to expect that state and local health departments will be able to address them all in isolation. Rather, effectively reducing the anticipated adverse effects will require a wide range of actions to be undertaken by both private and public actors across the state. For example, private businesses and households likely will implement many adaptation activities—such as adopting air conditioners, air filters, and back‑up power generation—to reduce their own risks. Similarly, local governments are likely to respond to climate threats by developing and implementing plans to protect their communities, such as by establishing additional cooling centers where residents can gather during heat waves. Moreover, a wide variety of state departments that do not directly work on health policy already are taking and will continue to take actions to reduce climate risks, such as urban greening projects to provide shade and reduce heat islands, improved forest management activities to reduce the severity of wildfires, and water management projects to address drought‑related water shortages. All of these programs can help reduce climate impacts on health, but they are mostly implemented through the state’s natural resource and environmental protection departments, rather than through state health departments.
Within this broader context of public and private adaptation actions, the Legislature may want to consider what role state health programs and policies can and should play in adapting to climate change, including how they interact with local adaptation activities. Below, we discuss some of the key climate‑related issues that state health policymakers and departments might wish to consider. The broad categories of activities include (1) assessing and addressing existing data and analysis gaps, (2) providing support and coordination for efforts at the local level and across state government, (3) focusing on the disproportionate needs of vulnerable populations, and (4) ensuring the health care delivery system is adequately prepared.
How Can the State Improve Monitoring and Analyses of Health Effects? The Legislature will want to consider what additional data regarding climate change impacts on health the state needs to inform its responses. First, the Legislature could consider opportunities to improve the state’s ongoing monitoring of current health effects related to climate change. For example, the state currently does not have a surveillance system for monitoring the real‑time health effects of extreme heat in California, including when and where heat‑related deaths and injuries are occurring. Health outcomes—such as deaths and emergency room visits—are not collected in real time, and the official data likely underestimate the number of deaths related to extreme heat. Addressing this deficiency also will require better linking and sharing of public health and health care delivery data across health plans, providers, facilities, labs, and state and local agencies. Similarly, the state currently lacks the ability to comprehensively monitor the overall health effects from exposure to wildfire smoke. For example, existing official air quality monitoring networks often are not sufficiently dense to measure the effects of smoke on ambient air quality at the local level, and relevant health outcome data is not easily accessible or available in real time. Establishing better systems for monitoring the effects of climate‑related health outcomes could help policymakers better assess the current magnitude of these health effects and identify trends that merit additional policy action.
Second, there is limited quantitative information available about the degree to which climate change is projected to impact future health outcomes in California, such as illnesses, injuries, and deaths. Based on our initial review, the available studies only rarely focus on California‑specific effects and generally concentrate on past events or explore only a limited set of climate‑related health outcomes. For example, only very limited information is available on the projected impact of wildfire smoke on various illnesses (such as asthma) and the impact of additional disasters on behavioral health conditions. In addition, there is very little detail about the health effects of climate change—rather than the frequency or severity of disaster events—on specific communities and populations. The state could consider ways to support future efforts to (1) make health outcome data more accessible to researchers, (2) consolidate and summarize the available academic research on the magnitude of the potential future health outcomes, and (3) support additional analyses of future climate‑related health outcomes in California. Better forecasts of future health outcomes in California could help determine the scope of policy action that might be warranted, prioritize the climate impacts on which the state should focus, and help the state strategize about potential options and align the necessary fiscal resources for addressing the likely health effects.
How Can the State Evaluate Which Adaptation Strategies Best Reduce Health Risks? In addition to assessing and addressing existing data gaps for climate‑related health impacts, the Legislature also faces the challenge of evaluating the effectiveness of potential strategies to respond to those impacts. Currently, only limited information is available on which adaptation strategies are likely to reduce future health risks at the lowest possible costs, and how equitably the benefits and costs of those strategies are distributed across different regions and populations. For example, which strategies reduce heat‑related mortality cost‑effectively is still unclear, making it difficult for the Legislature to determine whether to prioritize funding for expanding the urban tree canopy, additional cooling centers, subsidies to purchase or run air conditioning, public education campaigns, or other strategies. To address these gaps, the Legislature could consider supporting additional research and pilot projects to evaluate a variety of different adaptation strategies. This information could then be used to (1) prioritize funding for future adaptation programs, (2) compare the health benefits of climate‑focused programs to other programs that might improve health outcomes (such as separate efforts to improve the state’s Medi‑Cal system), and (3) provide technical assistance to local governments that are exploring opportunities to reduce future climate‑related health risks.
How Can the State Support Local Health Programs? Since climate impacts will vary by region and community, maintaining a strong role for regional and local decision‑making will help ensure adaptation activities are addressing the most pressing climate impacts in each area. In addition, local governments currently play a critical role in implementing key health programs, such as local public health programs and behavioral health services. However, most local public health departments lack in‑house and local expertise on assessing and responding to the impacts of climate change, which limits their ability to advise and assist local residents, businesses, and health providers. In addition, some of these departments may not have enough staff to support and manage data collection and reporting, limiting real‑time surveillance. As such, the Legislature will want to consider how the state can support these local health programs as they respond to the challenges posed by climate change. Some potential areas of focus could include:
- Conduct Research on Local Climate Impacts. While certain existing state efforts—such as CalBRACE, the California’s Fourth Climate Change Assessment, and Cal‑Adapt—provide some region‑specific climate information, the state could support additional efforts to provide more detailed information on local health outcomes to inform local decision‑making and prioritization. Local efforts also could be informed by the state conducting evaluations of which adaptation strategies best reduce climate‑related health risks, as discussed above.
- Technical Assistance. The Legislature could increase mechanisms to provide state‑level guidance and expertise to support activities at the local level. For example, this could include providing guidance on best practices to help local governments determine which adaptation interventions to pursue. It also could include funding additional staff with expertise in climate change impacts and adaptation strategies at CDPH explicitly to provide technical assistance to local health departments. (CDPH recently helped the San Diego Health and Human Services Agency in developing a climate change and health plan and implementing a variety of other climate‑related activities, but the department indicates that the six staff in its Climate Change and Health Equity Section have limited capacity to respond to requests for such assistance.)
- Financial Support. The Legislature could provide additional funding to local public health departments. Additional state support could help local agencies fill some of their existing expertise and capacity deficiencies. The 2021‑22 budget agreement between the Legislature and Governor committed $300 million in ongoing General Fund beginning in 2022‑23 for public health “infrastructure” (such as staffing, lab capacity and equipment, and information technology systems) at the state and local levels. The Legislature could consider directing a portion of this funding specifically to address climate‑related gaps.
How Can State Health Departments Support and Coordinate With Other State Agencies? Given the crosscutting nature of climate change impacts and the many state departments that will be involved, the Legislature may want to ensure that state‑level efforts are coordinated and informed by health experts. In particular, the Legislature could require that the expertise in the state’s health agencies is being used to inform the design of climate adaptation programs and regulations in other agencies that might lack such expertise. Some examples of such interagency consultation already exist. For instance, CDPH is providing technical assistance to the California Division of Occupational Safety and Health in its efforts to develop and adopt workplace heat standards. Similar types of efforts from other non‑health state departments likely will be considered in future years, such as potentially establishing heat or smoke safety standards for outdoor activities at schools, updating building codes, or making changes to general planning requirements. As more agencies begin to implement programs meant to reduce adverse health effects from climate change, the Legislature could consider adding a requirement that the administering department consult with CDPH when developing those programs’ regulations or guidelines.
How Can the State Help Reduce Impacts on the Most Vulnerable Populations? As discussed above, certain populations—such as low‑income households and medically sensitive populations—generally are more vulnerable to the effects of climate change. Targeting state programs in ways that support these vulnerable populations could help address some of the most significant adverse health effects of climate change, as well as reduce the inequitable distribution of impacts. This could include steps such as establishing programs that provide free or low‑cost air filters or masks to low‑income populations, and ensuring warnings about extreme heat and air quality are translated and targeted to reach medically and/or socially vulnerable populations. In addition, given that Medi‑Cal provides coverage to 14 million Californians with low incomes—many of whom likely are disproportionately vulnerable to climate change—the Legislature could consider the system’s role in addressing and preventing climate‑related adverse health impacts. For example, the Legislature could expand Medi‑Cal’s role in providing nonmedical benefits that address the negative health impacts of climate change, such as by standardizing the provision of air conditioners and asthma remediation services as Medi‑Cal benefits when medically necessary. (Currently, Medi‑Cal plans are not required to provide these benefits, but have the option to do so.) Additionally, the Legislature could consider strengthening Medi‑Cal managed care plans’ role in helping their members prepare for and navigate services during and after emergencies. For example, the state could consider putting in place additional policies requiring managed care plans or their contracted providers to work more directly with their most vulnerable members during emergencies.
How Can the State Ensure the Health Care Delivery System Is Adequately Prepared? The Legislature could consider steps to ensure the state’s health care delivery system is adequately prepared for the impacts of climate change. For example, the Legislature could consider requiring that providers receive more training on emerging conditions and diseases. Additionally, because managed care plans arrange and pay for the health care of most (around 26 million) Californians, ensuring they are well equipped to identify and address climate‑related health risks will be an essential component of an effective statewide strategy. Given the role the Legislature plays in setting policies for managed health care plans, it can help ensure the impacts of climate change are adequately incorporated in those policies. For example, the Legislature currently provides input on what data the plans must make available to state regulators. The Legislature could consider adding new data submission requirements on measures related to the health impacts of climate change to facilitate statewide tracking of impact trends and guide state‑level responses.
Conclusion
Climate change already is having adverse health impacts across the state, and these impacts are projected to grow over the coming decades. The weight of these burdens will not be spread uniformly across the state. Rather, some regions are disproportionately susceptible to climate‑induced events and less able to adapt, and certain individuals face greater vulnerability due to their underlying health status, age, means, type of work, or other characteristics. The more the state can learn about these adverse health impacts and which interventions are most cost effective, the better positioned it will be to prepare, plan ahead, and minimize these inevitable impacts.
