Will Owens
March 6, 2025
The 2025-26 Budget
CalAIM Enhanced Care Management and Community Supports Implementation Update
- Introduction
- Background
- ECM and Community Supports Implementation
- Summary of Utilization Data and Key Trends
- LAO Analysis of Utilization Data
- Issues for Legislative Consideration
Summary
Medi‑Cal Waiver Intended to Improve Care for High‑Cost, High‑Need Members. Medi‑Cal provides health care coverage to almost 40 percent of Californians, but the program’s complexity makes it difficult for some individuals to access appropriate care. The state received federal approval for the California Advancing and Innovating Medi‑Cal (CalAIM) waiver that, in part, allows the state to draw down additional federal funding for two new benefits: Enhanced Care Management (ECM) and Community Supports. These benefits are provided by managed care plans (MCPs) and are intended to provide cost‑effective services to high‑cost, high‑need Medi‑Cal members to improve health outcomes and reduce reliance on more costly medical services. The ECM benefit provides personalized care management to eligible members and Community Supports services—largely of a social services nature—are substitutes to traditional, often more costly, medical services. Members may be eligible for both benefits, as the two benefits serve broadly overlapping populations. However, the overlap is limited by the fact that each of the ECM benefit and the 14 Community Supports services has distinct eligibility criteria.
ECM and Community Supports Utilization Lower Than Expected, but Has Grown in Recent Years. The Department of Health Care Services (DHCS) has estimated that between 3 percent and 5 percent of all MCP members statewide are potentially eligible for ECM, but no such estimate exists for Community Supports. (One reason there is no eligibility estimate for Community Supports is that the eligibility rules for varying Community Supports benefits are different making estimating the eligible population challenging.) The percent of MCP members statewide utilizing ECM and Community Supports in 2022 was 0.6 percent and 0.1 percent, respectively, with both increasing to 0.9 percent in 2024. The complexities of integrating social service providers into MCP networks as well as broader systemic constraints that may limit the provision of services appear to be the main factors keeping utilization lower than expected.
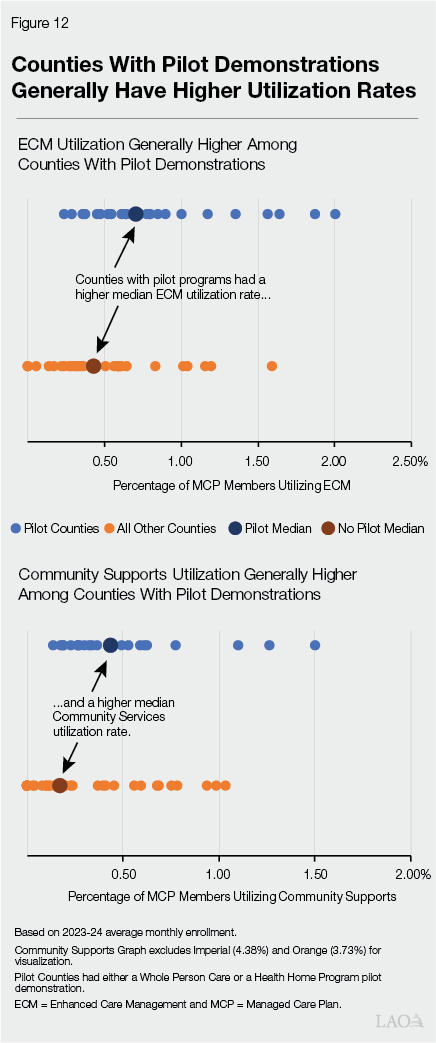
Utilization Varies Across Counties and MCPs Due to a Variety of Factors. Benefit utilization rates across counties and MCPs vary considerably, with generally lower utilization rates in the central and eastern portions of the state. Underlying differences in the eligible populations across the state may partially explain some of the regional variation in utilization. In addition, counties that had a related pilot demonstration under the prior Medi‑Cal waiver tend to have higher utilization rates than counties that did not. Variation across MCPs may also be due to differences in available provider networks and overall implementation of the program.
More Information Needed to Monitor and Assess Waiver. We recommend the Legislature consider requesting additional information from DHCS to enable it to (1) assess whether benefit utilization will continue to grow; (2) assess possible future state costs; (3) understand the variation in utilization across MCPs and counties; (4) identify barriers that MCPs face to increasing access to the benefits; and (5) ensure that a system is in place to allow for a robust, ongoing evaluation of the cost‑effectiveness of the benefits and their impact on health outcomes. DHCS will complete evaluations of certain components of the CalAIM waiver by the end of 2025, which will provide some of the information noted above.
Introduction
This report assesses the implementation of the ECM and Community Supports benefits within the CalAIM federal waiver as reported by the utilization data from DHCS. This report begins with background information on the Medi‑Cal program as well as the challenges in providing services to the state’s high‑need, high‑cost Medi‑Cal members. Next, we identify and assess key trends in the ECM and Community Supports utilization data and consider reasons for variations across the state. We then provide the Legislature with issues to consider and questions for the administration as the state evaluates program outcomes and prepares to renew its federal waiver, which expires in December 2026.
Background
Medi‑Cal Provides Health Care Services to Low‑Income Californians
Medi‑Cal Provides a Range of Health Care Services. Medi‑Cal, the state’s Medicaid program, provides health care coverage for low‑income Californians. Historically, Medi‑Cal has covered traditional health care services such as visits to the doctor’s office, stays at the hospital, prescription drugs, behavioral health services, long‑term care, and dental services, among many other areas. The Governor’s budget assumes an average monthly Medi‑Cal caseload level of 15 million in 2024‑25, almost 40 percent of Californians.
Medi‑Cal Is a State‑Federal Partnership. A key component of Medi‑Cal, and the Medicaid program as a whole, is the shared programmatic and fiscal responsibility between California and the federal government. The federal government has a number of program requirements that Medi‑Cal must follow in order to receive federal funding for eligible services. However, the state is allowed certain flexibilities in how to structure the Medi‑Cal program that enable it to receive additional federal funding for certain services.
Medi‑Cal Is a Sizeable Portion of California’s Budget. More than half of Medi‑Cal’s budget is supported by federal funds, with the remainder supported by the General Fund and other state and local government sources. The General Fund portion of Medi‑Cal comprises a sizable share of overall state General Fund spending, ranging between 13 percent and 17 percent in most of the last ten years. As a share of General Fund spending, Medi‑Cal is the state budget’s second largest program after schools and community colleges.
Medi‑Cal Services Provided Through a Variety of Delivery Systems. The primary way Medi‑Cal delivers services to beneficiaries is by contracting with health insurance plans, also known as MCPs, which serve the majority of enrollees. The state provides MCPs monthly payments to enroll Medi‑Cal beneficiaries, while the plans in turn are required to arrange for the health care of their enrollees. Medi‑Cal pays for some health care services, such as pharmacy benefits, by reimbursing providers directly—known as the fee‑for‑service delivery system. Additionally, counties serve as distinct delivery systems both for treatment to Medi‑Cal enrollees with severe mental health conditions and for personal care services.
Medi‑Cal’s Complexity and High‑Need, High‑Cost Populations Pose Challenges
Medi‑Cal’s Complexity Puts Burden on Beneficiaries and Program Administrators. The complexity of the Medi‑Cal program impacts both beneficiaries and the state in its oversight and administration of Medi‑Cal. Historically, Medi‑Cal benefits have not always been provided through the same delivery system in all parts of the state, and not all benefits have been available everywhere in the state. To some extent, this variation reflects past efforts to test new models of care in only portions of the state. Depending on which services beneficiaries require, they may need to navigate multiple delivery systems, which can make it difficult for beneficiaries to receive all the services that their conditions would indicate are needed. Difficulties navigating Medi‑Cal’s multiple systems can be particularly pronounced for individuals with multiple complex conditions.
Disproportionately High Share of Services Costs Provided to a Relatively Small Number of High‑Need Beneficiaries. Medi‑Cal enrollees are diverse and have varying health statuses. The cost of Medi‑Cal services per enrollee varies significantly and a small number of Medi‑Cal enrollees account for a large and disproportionate share of total spending in Medi‑Cal. A 2014‑15 analysis by DHCS showed the most costly 1 percent of Medi‑Cal enrollees accounts for about 20 percent of program spending and the most costly 20 percent of Medi‑Cal enrollees account for about 70 percent of program costs. Past research indicates that the highest‑cost enrollees typically are being treated for multiple chronic conditions (such as diabetes or heart failure) and often have mental health or substance use disorders. Costs for this population often are driven by frequent hospitalizations and high prescription drug costs. In some cases, social factors like homelessness play a role in the high health care utilization of these enrollees. Costs are also high for individuals residing in long‑term care facilities, which could potentially increase in coming years as the state’s population ages.
Federal Medicaid Waivers Allow Testing New Approaches
State Has Flexibility to Change Medi‑Cal Service Delivery Through Federal Waivers. Federal law lays out many basic requirements for how states may operate Medicaid programs and requires states to offer certain benefits. Federal law also allows the federal government to waive certain Medicaid requirements in some cases. States often take advantage of federal waivers to provide Medicaid benefits in new ways and, in some cases, obtain funding for services that might not otherwise be available.
California Pilot‑Tested Two Programs to Address the High‑Need, High‑Cost Population Challenge. Under the state’s prior Medi‑Cal waivers, the state piloted two programs (from 2016 through 2021) that focused resources and attention on the highest‑risk, highest‑needs beneficiaries, often with the intent to prevent the worsening of severe health conditions. The first, the Whole Person Care (WPC) program, was a set of local pilot programs—typically run by county health agencies—to coordinate physical health, behavioral health, and social services for beneficiaries with the highest levels of need and/or risk. Each local WPC pilot determined target populations—among a predetermined set which included, for example, high utilizers of services and homeless individuals—and developed strategies to tailor service delivery to those groups. The second, the Health Home Program (HHP), had similar goals to the WPC program and provided extra services—including care management—to Medi‑Cal beneficiaries who suffered from chronic health and/or mental health conditions that result in high use of health care services.
Evaluation of Pilot Programs Found Participants Had Lower Costs and Emergency Department Utilization. As required by the federal waiver, DHCS contracted with the University of California, Los Angeles to perform evaluations of WPC and HHP to determine if the programs improved health outcomes. Patients who received services under WPC or HHP generally saw a reduction in emergency department visits and hospitalizations, along with overall lower health care costs due to lower utilization of certain services. Additionally, patients increased utilization of certain outpatient services, like primary care, immediately following enrollment in a pilot program. However, after accessing the necessary services to meet their immediate medical needs, those same patients reduced their utilization of those services, further decreasing health care costs.
The CalAIM Waiver Demonstration
CalAIM Intended to Address Challenges of Complexity and High‑Need, High‑Cost Populations. At a high level, CalAIM is intended to address some of the challenges previously identified by (1) providing more comprehensive benefits and services to high‑need, high‑cost populations and (2) streamlining and standardizing Medi‑Cal benefits and administration. Our office assessed the entire CalAIM waiver when it was first proposed in the Governor’s 2020‑21 budget proposal, but implementation was delayed due to the onset of the COVID‑19 pandemic. Our office performed a number of follow‑up assessments when CalAIM was introduced again in the Governor’s 2021‑22 budget proposal. While CalAIM consists of a number of program changes across the Medi‑Cal system, this post will focus on two key components of the waiver, ECM and Community Supports.
ECM and Community Supports Reflect an Increased Focus on High‑Need, High‑Cost Populations. ECM and Community Supports are benefits administered by MCPs that were modeled off of the state’s experience with the WPC and HHP pilots under the previous federal waivers. The overall goals of both ECM and Community Supports include improving health outcomes, providing cost‑effective benefits that reduce the need for higher‑cost medical services, and improving care coordination and access among members. (Other components of CalAIM are intended to reduce the complexity of the system itself, such as by streamlining and standardizing Medi‑Cal benefits and administration.)
- ECM Benefit Provides Care Coordination to Highest‑Need Medi‑Cal Members. ECM is intended to be a comprehensive, whole‑person care management benefit that coordinates all aspects of a member’s care across physical and behavioral health delivery systems. Each eligible member is assigned a personal ECM Care Manager who helps to identify all resources to address all needs of the member, including the development of a care management plan.
- Community Supports Provide Medically Appropriate and Cost‑Effective Substitutes for Other Covered Services. Figure 1 provides a full list of the currently approved Community Supports along with a brief description. Community Supports are services or settings—largely of a social services nature—that can substitute for, and potentially decrease utilization of, a range of covered Medi‑Cal benefits, such as hospital care, nursing facility care, and emergency department use. For example, a member may receive home modifications that would allow them to remain in their home rather than need to move to an assisted living facility (which has a much higher cost to the state).
Figure 1
Available Community Supports Services
|
Benefit |
Description |
|
Housing‑Related Services (“Housing Trio”) |
|
|
Housing transition navigation services |
Assistance with obtaining housing. This may include assistance with searching for housing or completing housing applications, as well as developing an individual housing support plan. |
|
Housing deposits |
Funding for one‑time services necessary to establish a household, including security deposits to obtain a lease, first month’s coverage of utilities, or first and last month’s rent required prior to occupancy. |
|
Housing tenancy and sustaining services |
Assistance with maintaining stable tenancy once housing is secured. This may include interventions for behaviors that may jeopardize housing, such as late rental payment and services, to develop financial literacy. |
|
Recuperative Services |
|
|
Recuperative care (medical respite) |
Short‑term residential care for beneficiaries who no longer require hospitalization, but still need to recover from injury or illness. |
|
Respite services |
Short‑term relief provided to caregivers of beneficiaries who require intermittent temporary supervision. |
|
Short‑term, post‑hospitalization housing |
Setting in which beneficiaries can continue receiving care for medical, psychiatric, or substance use disorder needs immediately after exiting a hospital. |
|
Sobering centers |
Alternative destinations for beneficiaries who are found to be intoxicated and would otherwise be transported to an emergency department or jail. |
|
Services to Enable Members to Remain in a Home‑Like Setting |
|
|
Day habilitation programs |
Programs provided to assist beneficiaries with developing skills necessary to reside in home‑like settings, often provided by peer mentor‑type caregivers. These programs can include training on use of public transportation or preparing meals. |
|
Nursing facility transition/diversion to assisted living facilities |
Services provided to assist beneficiaries transitioning from nursing facility care to community settings, or prevent beneficiaries from being admitted to nursing facilities. |
|
Nursing facility transition to a home |
Services provided to assist beneficiaries transitioning from nursing facility care to home settings in which they are responsible for living expenses. |
|
Personal care and homemaker services |
Services provided to assist beneficiaries with daily living activities, such as bathing, dressing, housecleaning, and grocery shopping. |
|
Environmental accessibility adaptations |
Physical adaptations to a home to ensure the health and safety of the beneficiary. These may include ramps and grab bars. |
|
Medically tailored meals |
Meals delivered to the home that are tailored to meet beneficiaries’ unique dietary needs, including following discharge from a hospital. |
|
Asthma remediation |
Physical modifications to a beneficiary’s home to mitigate environmental asthma triggers. |
Eligibility for ECM and Community Supports Differ. ECM and Community Supports are two distinct types of benefits that are intended to be complementary, with both reducing the reliance on high‑cost medical services while improving health outcomes. However, not all individuals who are eligible for ECM are eligible for Community Supports, or vice versa.
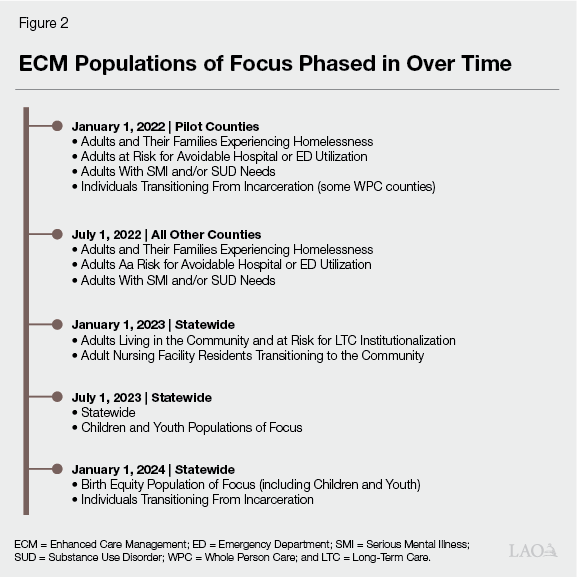
- ECM Is a Required Benefit for All Eligible MCP Members of Populations of Focus (POFs). The ECM benefit is required to be offered by MCPs to all members if they meet the eligibility requirements of any of the specified POFs. The number of POFs have increased overtime and include populations such as individuals experiencing homelessness, individuals at risk for hospitalization, and individuals with a serious mental illness or substance use disorder. Due to the specific eligibility requirements, many MCPs are able to identify members who may be eligible for ECM services based on administrative data. Members may be eligible for ECM based on one or multiple POFs, but ultimately must agree to receive the benefit and participate in the program.
- Community Supports Eligibility Is More Complex and Is an Optional Benefit. Community Supports services are optional benefits that MCPs may choose to offer, and each of the 14 Community Supports (as listed in Figure 1) can have very different eligibility criteria. Community Supports services are often based not only on a member’s characteristics (for example, an individual at risk for or experiencing homelessness), but on the specific medical and social service needs of the member. For example, while two members may share similar economic and health conditions, if one is transitioning from incarceration they may be eligible and have needs for a different set of Community Supports than another who is trying to remain in their home instead of being placed in a nursing facility. Both members would be eligible for Community Supports, but the specific Community Supports they would receive would be tailored to their individual needs. These complex and varying circumstantial eligibility requirements make it difficult to determine the total number of members potentially eligible for Community Supports services statewide. Similar to ECM, members must agree to receive the benefit and participate in the program to access the services.
Waiver Requires Evaluation of Outcomes. As a part of the approved CalAIM waiver, DHCS is required to evaluate the cost‑effectiveness of Community Supports during the term of the waiver and submit interim and final evaluations to the federal government by December 2025 and December 2028, respectively. The ECM benefit, which was closely related to many of the components of the WPC and HHP pilots, was previously determined to be cost‑effective and is not required to undergo a full evaluation like Community Supports. DHCS will also release an evaluation, required by the waiver, of the Providing Access and Transforming Health (PATH) initiative (we describe PATH—which provides funding to help providers participate in CalAIM—in more detail in subsequent sections) to determine if the additional funding strengthened ECM and Community Supports infrastructure and increased benefit utilization. As the interim evaluations will not become available until later this year, we have begun to evaluate the data currently available from the department to provide the Legislature an update on the implementation of ECM and Community Supports and raise issues for legislative consideration.
ECM and Community Supports Implementation
ECM Recipients
MCPs Phased in ECM to Different POFs Over Time. As shown in Figure 2, MCPs have been required to provide the ECM benefit to members based on a list of eligible POF categories that have grown over time. These POFs are intended to direct the benefit to members who would especially benefit from personalized care coordination, such as individuals at risk for avoidable hospitalization or emergency department utilization. Most POF eligibility criteria include some combination of a complex physical or mental health condition along with a social or environmental factor that influences their health. Many of the POFs are also similar to the targeted populations within the WPC and HHP pilots. Based on a one‑time analysis of actuarial data, DHCS estimated that between 3 percent and 5 percent of all MCP members were eligible for the ECM benefit under at least one POF. Some MCPs indicated that potential eligibility ranged from 3 percent to as high as 7 percent of their membership.
DHCS Implemented a Number of Program Changes to Increase Access to ECM. In 2023, DHCS implemented a number of policy changes intended to make it easier for members to access ECM services, including (1) preventing MCPs from imposing additional eligibility requirements for ECM authorization, (2) requiring MCPs to contract with ECM providers that specialize in each POF and have an existing footprint in the communities they serve, and (3) limiting reassessments of eligibility by MCPs. Beginning in 2025, DHCS has implemented a standardized ECM referral form (including restricting MCPs from requesting additional information) and required MCPs to implement presumptive eligibility for members referred by authorized ECM providers. (The ECM program changes made in 2025 will not be reflected in our assessment and could increase utilization of the ECM benefit.)
Community Supports Services
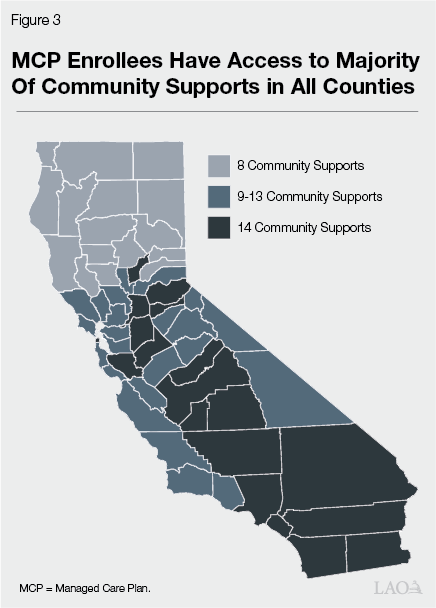
MCPs Have Expanded the Number of Community Supports Available Over Time. Community Supports are an optional benefit that MCPs may offer to eligible members. When Community Supports first became available in January 2022, only five Community Supports were offered by at least half of all MCPs and only two MCPs offered all Community Supports. MCPs have been offering more Community Supports since they first became available. As of June 2024, there are seven MCPs offering all Community Supports that represent 44 percent of the state’s total MCP enrollment. As shown in Figure 3, all counties have at least eight Community Supports offered by at least one MCP and there are 19 counties where all Community Supports are available from at least one MCP. Unlike with ECM, there is no statewide estimate of potential eligibility for each Community Support. Each Community Support has very different eligibility criteria which makes it difficult to estimate the total number of individuals eligible for each service. For example, for an individual to receive the Medically Tailored Meals benefit they must have a chronic condition and have been discharged or be at risk of placement in a hospital or skilled nursing facility. For the same individual to receive Day Habilitation services, they must also be experiencing or at risk of experiencing homelessness and who’s housing stability would be improved by the service. Without comprehensive, real‑time, administrative data, it would be difficult to estimate the number of MCP members who would be eligible for both of these services.
DHCS Reversed an Initial Flexibility Afforded MCPs to Improve Access to Community Supports Services. Prior to the launch of the Community Supports benefit, DHCS allowed MCPs to modify or restrict Community Supports service definitions if their anticipated provider network would not allow for the countywide provision of the benefit. This flexibility could include changes to the scope of services or the eligibility of members. MCPs would then have three years to expand their provider network and capacity. DHCS later determined that the allowed modifications created barriers to implementation and accordingly required all MCPs to meet the DHCS‑established service and eligibility definitions by January 1, 2024.
ECM and Community Supports Funding
ECM and Community Supports Funded Within MCP Rates. The state pays MCPs a monthly rate for each enrollee based on plans’ past expenditures, as well as adjustments for inflation and other factors determined by actuaries. The ECM and Community Supports benefits are included in this actuarial calculation, and it is up to MCPs to arrange for ECM and Community Supports services for their enrolled members through the plans’ network of providers. MCPs contract with providers to reimburse for ECM and Community Supports services and can structure reimbursements in different ways.
State Provides Grants to MCPs and Providers to Develop ECM and Community Supports Program Infrastructure. In order to support the implementation of ECM and Community Supports, the state implemented the PATH initiative and the Incentive Payment Program (IPP) to help create and expand program infrastructure.
- PATH Initiative Provides Funding to Help Providers Participate in CalAIM. The state received approval under the waiver to provide $1.85 billion in total funds (incorporating the federal match) for the PATH initiative. PATH consists of multiple initiatives intended to build up the capacity and infrastructure of CalAIM providers. This was needed as these providers were not traditionally part of the health care delivery system. To support ECM and Community Supports services, PATH provides funding for (1) a virtual marketplace for technical assistance; (2) regional facilitators to support collaborative planning efforts among MCPs, providers, and other behavioral health organizations; and (3) Capacity and Infrastructure Transition, Expansion and Development (CITED) grants that provide direct funding to providers. PATH CITED grants could be used to hire and train staff; expand service capacity; or improve organizational infrastructure, such as upgrading information technology systems. In addition, the state provided an additional $40 million General Fund to support ECM and Community Supports capacity in clinics.
- IPP Provides Additional Funding to MCPs to Expand Provider Network and Expand Access to Community Supports. The state received approval under the waiver to provide $1.5 billion in total funds (incorporating the federal match) as incentive payments to MCPs. To receive funding, MCPs submit data to demonstrate they are meeting certain performance measures on ECM and Community Supports implementation. MCPs have flexibility in how they use IPP funds. For example, this funding can be used to hire and train staff, provide technical assistance to providers, or provide supplemental payments to providers to incentivize participation in ECM and Community Supports.
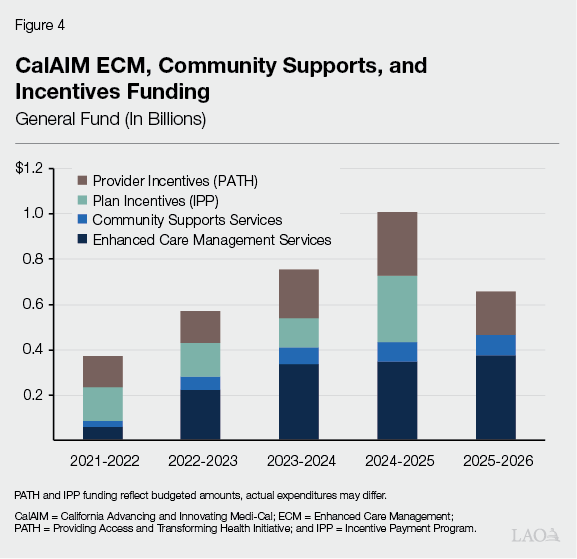
Funding Has Increased Over Time as More Beneficiaries Access ECM and Community Supports. The Governor’s 2025‑26 budget proposes ECM spending at $956 million (total funds) and Community Supports spending at $231 million (total funds), a $67 million (7.5 percent) and $11 million (5 percent) increase over revised 2024‑25 levels, respectively. The General Fund share of the ECM and Community Supports benefit is approximately 40 percent. As shown in Figure 4, General Fund spending for these programs has increased substantially since 2021‑22, with ECM spending increasing by $308 million (466 percent) and Community Supports spending increasing by $68 million (317 percent). Both IPP and PATH—incentives funding that is also shown on Figure 4 in addition to General Fund ECM and Community Supports spending—have fixed, limited‑term funding availability that ends in 2025‑26 and 2026‑27, respectively.
Summary of Utilization Data and Key Trends
ECM and Community Supports Quarterly Implementation Report Provides Benefit Utilization Data. DHCS publishes quarterly implementation monitoring reports that include data on the utilization of the ECM and Community Supports benefits across the state, broken down by MCP and county. The reports also contain high‑level provider information by each MCP, including the number of provider contracts and the type of providers (for example, whether the provider is a Federally Qualified Health Center or an organization that serves individuals experiencing homelessness). One key component of the report is the “utilization rate” for both ECM and Community Supports. This rate is calculated as the share of Medi‑Cal managed care members who have enrolled in ECM or have utilized at least one Community Support. Our assessment of ECM and Community Supports utilization draws from data published in this report which, at the time of this brief, spans from January 2022 to June 2024.
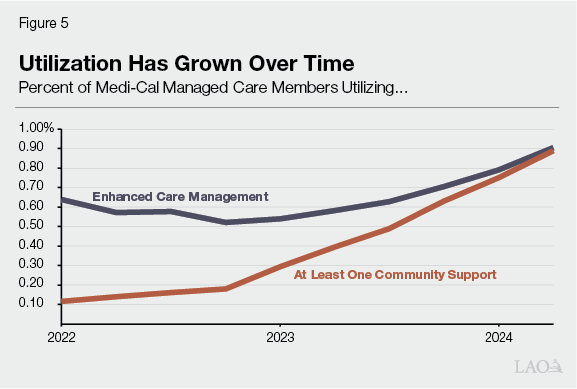
Benefit Utilization Has Been Low, but Steadily Growing. As Figure 5 shows, both ECM and Community Supports utilization began relatively low during the initial period when the benefits became available. Initially, ECM utilization started much higher than Community Supports, though the gap has narrowed in recent years. This initial gap is somewhat expected as the previous WPC and HHP pilot demonstrations provided services most similar to those in ECM, so plans were better able to transition to providing the ECM benefit. Utilization rates across the state were relatively flat until 2023, when ECM utilization began to gradually increase and Community Supports utilization increased much more quickly.
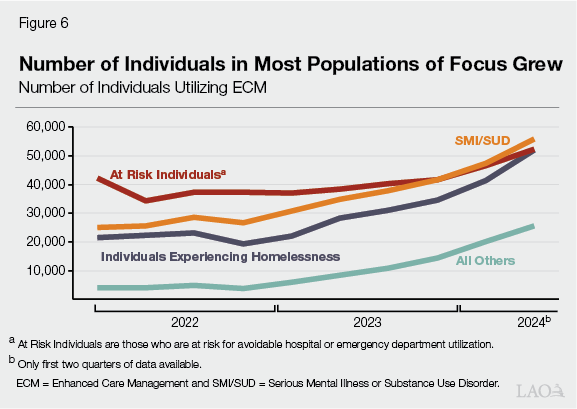
Majority of ECM Participants Qualify Under Three POFs. MCP members may be eligible for ECM under multiple POFs, but as shown in Figure 6, the three most common POFs that members have qualified under are individuals experiencing homelessness, individuals at risk for hospitalization, and individuals with a serious mental illness or substance use disorder. All three of these POFs were some of the optional target populations available for WPC and HHP pilot demonstrations, so participating MCPs had already identified providers who would be able to provide services to these populations.
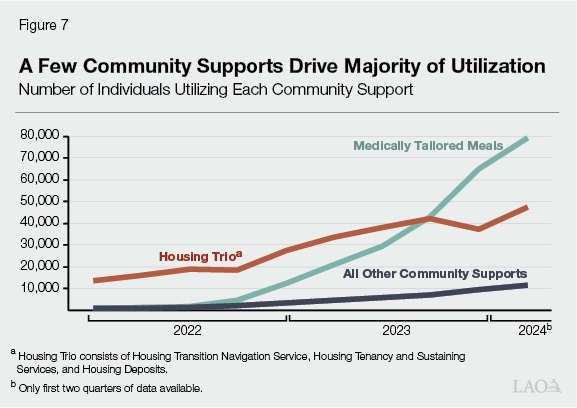
Medically Tailored Meals and Housing Trio Were Most Utilized Community Supports. Figure 7 shows Community Supports utilization has grown in recent years, though the majority of growth is concentrated in a handful of services. Medically Tailored Meals is the most utilized Community Support by a fairly large margin. However, this is driven primarily by utilization within two health plans in two counties. CalOptima health plan in Orange County accounts for almost one‑third of all Community Supports utilization statewide, with the majority of those services being Medically Tailored Meals. Beginning in 2024, Community Health Plan Imperial Valley in Imperial County has also begun to rapidly increase the number of members receiving Medically Tailored Meals. The other set of Community Supports that have been the most utilized are the “housing trio” (as described in Figure 1). Among these housing‑related services, Housing Transition Navigation Services is almost three times more common than Housing Tenancy and Sustaining Services and Housing Deposits.
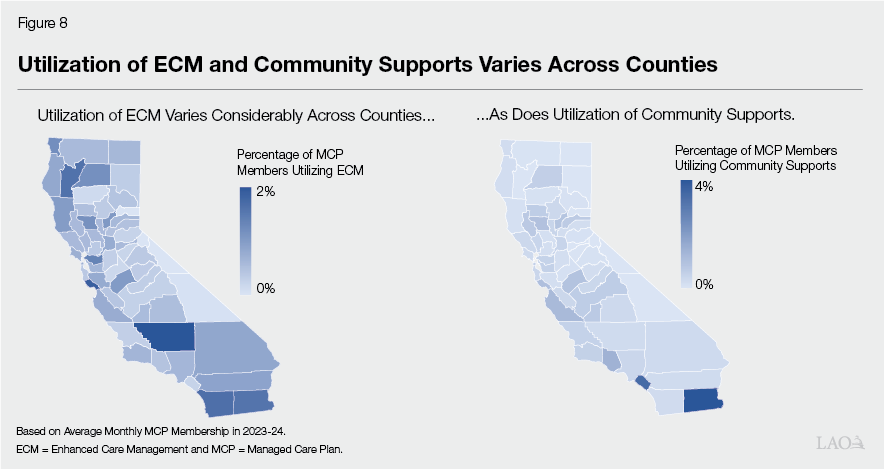
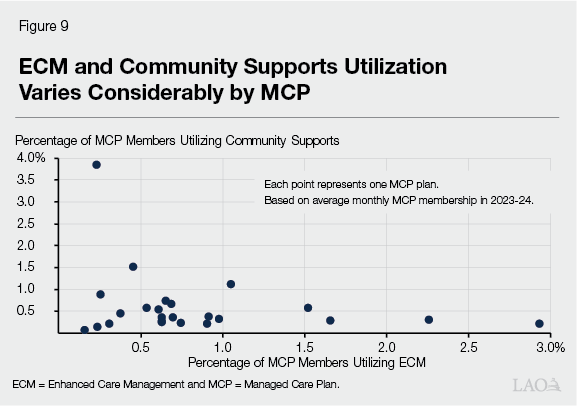
Participation Makes Up Small Share of Overall Medi‑Cal MCP Caseload, With Significant Variation Across Counties and MCPs. As shown in Figure 8, the utilization rates of both ECM and Community Supports are low in most counties, with the majority of counties having an ECM utilization rate below 0.6 percent of MCP members and a Community Supports utilization rate below 0.4 percent. The two outliers, as discussed above, are the high Community Supports utilization rates in Orange County (3.7 percent) and Imperial County (4.4 percent). Utilization rates across counties vary considerably, with generally lower utilization rates in the central and eastern portions of the state. Geographic differences can highlight regional differences in capacity or infrastructure, while differences across MCPs can also indicate differences in program implementation. As shown in Figure 9, most MCPs have less than a 1 percent utilization rate for both ECM and Community Supports. Even plans that have a higher utilization rate for ECM may have a low utilization rate for Community Supports, and vice versa.
LAO Analysis of Utilization Data
LAO Methodology. Our analysis consists primarily of an evaluation of the utilization data and provider information reported by DHCS in their quarterly implementation report. We also supplement our analyses with data reported by MCPs in their Housing and Homelessness Incentive Program submissions; responses to the California Health Care Foundation (CHCF) ECM and Community Supports implementor survey; and interviews with MCPs, ECM and Community Supports providers, counties, and DHCS.
Assessing Statewide Level of Utilization
Utilization Appears Low
Utilization of ECM Benefit Expectedly Lower Than Total Potential Eligibility. As shown earlier in Figure 5, the percent of MCP members statewide utilizing the ECM benefit was 0.6 percent in 2022, rising to 0.9 percent in 2024. Of particular note, only about one‑fifth of all MCP members that identified as homeless—a key POF—were receiving ECM services in 2023 (about 0.3 percent of all Medi‑Cal managed care members). As discussed above, DHCS had estimated that between 3 percent and 5 percent of Medi‑Cal MCP members were eligible for the ECM benefit. While the ECM benefit is intentionally targeted at a small subset of the overall Medi‑Cal population, the take up appears to be between about one‑third and one‑quarter of those eligible for services. As enrollees must agree to participate in ECM, participation may be impacted by enrollee interest. Given the notable variation between counties and MCPs, however, there likely are implementation differences—such as the availability of providers—leading to differences in take up.
Difficult to Assess Potential for Additional Growth in Community Supports Utilization. As also shown in Figure 5, the percent of MCP members statewide utilizing at least one Community Support was 0.1 percent in 2022, rising to 0.9 percent in 2024. As mentioned previously, there is no estimate for the total potential eligibility of MCP members for Community Supports, given the varying eligibility criteria among the 14 Community Supports services. That said, the differences across counties and plans indicate that, at least for some Community Supports, much higher utilization is possible. For example, the very high utilization rates of Medically Tailored Meals in two counties, by two plans using the same provider, may indicate more demand for the benefit above what is currently being provided.
Factors Possibly Limiting Utilization
Utilization May Continue to Grow, but Trend Uncertain. ECM benefit utilization started higher than Community Supports, in part due to the capacity established through the WPC and HHP pilot demonstrations, but remained stagnant for the first year and half of implementation. As plans, providers, and members have learned more about the benefit and DHCS made changes to policies to improve access to the benefit, utilization has increased. Community Supports utilization overall has steadily grown over the course of the demonstration. However, most of that growth has been concentrated among a few Community Supports services, and for other services utilization has been relatively flat or slightly declining. Limited data are available to evaluate the demand or capacity for additional services. As such, whether utilization will increase is unknown.
Three Key Factors May Be Limiting Utilization Statewide. Utilization of the ECM and Community Supports benefits appears to be lower than expected. Based on our analysis and conversations with MCPs and providers, we identify three key factors that appear to be driving lower utilization rates across the state.
- MCPs Have Limited Experience Offering Nonmedical Services. MCPs are responsible for arranging the majority of health care services their members need. While some plans may have offered certain care management or nonmedical benefits prior to CalAIM, ECM and Community Supports have required MCPs to expand their scope in terms of service offerings beyond what they have historically been responsible for. Most plans have received additional funding to assist in expanding their capacity to build provider networks to increase utilization of these new benefits. However, many plans have cited challenges in working with providers who are unfamiliar with how services are reimbursed within a MCP network.
- Providers Have Less Familiarity Working With MCPs. CHCF conducted a survey of MCPs and providers on CalAIM implementation in 2023 and again in 2024. While the survey samples were different, Figure 10 shows that two major factors for providers not participating in ECM and Community Supports remained the same in both years. Even three years into the program, unfamiliarity with the ECM and Community Supports benefits and how to provide them as a Medi‑Cal benefit are major challenges for providers to enter MCP networks. The difficulty MCPs have in adding ECM and Community Supports providers may be keeping utilization rates lower than expected.
- Systemic Constraints Limit Utilization. Lower‑than‑expected utilization of certain benefits may be driven more by systemic constraints across different regions of the state rather than a low demand for those benefits. Almost every MCP and relevant provider we spoke with cited the lack of available housing as a major challenge to providing the housing trio Community Supports. Members would remain eligible for the Housing Transition Navigation Services Community Support longer than anticipated as the lack of housing prevented placement. This in turn kept utilization of other Community Supports services, like Housing Deposits, lower than would be expected.
Figure 10
Top Reasons Providers Did Not Participate in
ECM or Community Supports
|
Reasons Given By Providers |
2023 Survey |
2024 Survey |
|
We are in the process of deciding whether to participate in ECM and/or Community Supports. |
✔ |
|
|
We are not sure how to participate in ECM and/or Community Supports. |
✔ |
✔ |
|
We do not have the capacity to meet the requirements of the program. |
✔ |
✔ |
|
We have heard that payment rates are too low. |
✔ |
|
|
Source: California Health Care Foundation and Goodwin Simon Strategic Research 2023 and 2024 Survey of CalAIM implementers. |
||
|
ECM = Enhanced Care Management. |
||
Potential Benefits of Increased Utilization
Possible That Utilization Will Continue to Increase. While utilization of ECM and Community Supports began lower than anticipated, the number of MCP members participating in the programs has steadily increased. As discussed, many of the factors limiting utilization may be addressed with time as familiarity with the program continues to grow. As shown in Figure 11, the total number of provider contracts for both ECM and Community Supports have increased over time as plans have worked to expand their networks. However, nontraditional providers are more than double the number of traditional providers in ECM and this ratio is even greater for Community Supports providers. Traditional providers are those that are typically within the MCP medical services network and would have experience working with MCPs to provide services and receive reimbursements (for example, Federally Qualified Health Centers, hospitals, and physician groups). Nontraditional providers typically provide social services, but may not have experience with MCPs to bill for those services (for example, community‑based organizations and organizations serving individuals experiencing homelessness). How quickly utilization will grow is hard to know because of the high concentration of nontraditional providers and the challenges cited above to incorporating providers more generally. Based on previous evaluations, increasing the number of Medi‑Cal members utilizing ECM could reduce overall health care costs, though cost‑effectiveness and improvements in health outcomes of Community Supports is still unknown.
Figure 11
Number of Contracts With Traditional
and Nontraditional MCP Providers
|
2023 Q3 |
2023 Q4 |
2024 Q1 |
2024 Q2 |
|
|
ECM |
||||
|
Traditional |
567 |
535 |
527 |
648 |
|
Nontraditional |
736 |
822 |
1,090 |
1,441 |
|
Community Supports |
||||
|
Traditional |
708 |
343 |
456 |
287 |
|
Nontraditional |
3,796 |
3,766 |
4,436 |
5,105 |
|
MCP = Managed Care Plan and ECM = Enhanced Care Management. |
||||
ECM Benefit Utilization Has Been Shown to Lower Costs and Improve Certain Health Outcomes. As highlighted earlier in the brief, the results from the evaluations of the WPC and HHP pilot demonstrations showed that participants generally saw a reduction in emergency department visits and hospitalizations, along with overall lower health care costs due to lower utilization of certain services. The results from the final evaluation focused on three primary target populations, which were equivalent to the ECM POFs of individuals experiencing homelessness, individuals at risk for hospitalization, and individuals with a serious mental illness or substance use disorder. Whether the ECM benefit will have the same overall level of cost‑effectiveness and positive health outcomes that were demonstrated in the pilots for additional POFs added under CalAIM is unknown. However, many new POFs may overlap with the three listed above and based on their eligibility criteria would still be considered high‑risk, high‑needs populations, and may still benefit from ECM enrollment.
Benefit of Increasing Utilization of Community Supports Unknown. The Community Supports program’s benefits to the state and Medi‑Cal members are currently being evaluated by DHCS. While the pilot demonstrations had the option to include nonmedical services within their pilots, it was not a key element of the pilot evaluation. Some MCPs cited the costs of providing Community Supports as higher than the payments received from DHCS. As MCPs continue to implement the Community Supports benefit, more information will be needed to determine what, if any, costs savings the state and MCPs are receiving in the form of lower utilization of more expensive medical services.
Significant Variation in Utilization Across Counties and MCPs
Many Factors Impact Variations in ECM and Community Supports Utilization. Some variation in utilization rates across counties and MCPs is expected as factors such as the differences in the concentration of POFs may drive some of the variation. In addition, there are capacity constraints for certain services that vary across the state and may impact utilization rates. There may also be differences in MCP characteristics that make them better equipped to implement the ECM and Community Supports benefits.
Variations in Extent of POFs Help Explain Some Variation in ECM Utilization Across Counties and MCPs. The ECM benefit is required to be offered by MCPs to individuals if they meet certain criteria for a POF. To the degree that plans have a varying share of members in each POF, it could lead to variations in utilization. For example, one county may have a disproportionate number of individuals experiencing homelessness or have a large number of individuals in skilled nursing facilities. However, more information on total potential eligibility by POF in each MCP would be needed to understand how much of the variation could be explained by differences in the underlying population characteristics.
Systemic Constraints, Such as Lack of Housing Supply, Vary Across State. While certain systemic constraints may be impacting utilization statewide, the effects and extent of those constraints may differ among counties and MCPs. While housing affordability and availability are major issues facing the state as a whole, certain regions may have a more acute housing shortage that would lead to lower utilization of certain Community Supports services. The availability of providers, especially nontraditional providers, may also lead to differences in benefit utilization across counties and plans. Certain regions have more community‑based organizations or community‑based organizations with sufficient resources to build the infrastructure needed to participate in a MCP network. Certain regions in the state with a limited number of social service providers prior to the ECM and Community Supports programs may lag in utilization of the benefits.
Counties That Were WPC or HHP Pilot Counties Have Higher Utilization Than Those Who Did Not. As described previously, the ECM and Community Supports benefits present challenges for both MCPs to implement as well as providers to participate in. As shown in Figure 12, however, counties that had a WPC or HHP pilot demonstration generally have a higher utilization rate than those counties that did not. MCPs in these counties had an opportunity to begin building provider networks and had first‑hand experience providing benefits similar to ECM and, possibly, Community Supports. The higher levels of utilization in pilot counties may indicate that utilization may increase as more time passes and MCPs and providers become more familiar with the program and build the necessary capacity to meet demand.
Providers Cite Grant Funding as Critical to Program Participation, but More Information Needed to Assess Impact. A number of providers we spoke with indicated that they would be unable to provide ECM and Community Supports services absent the support of the PATH program, both from the technical assistance provided and the direct grant awards. They cited the technical challenges of working within the MCP network, specifically around billing, and the need to hire individuals with experience in MCP reimbursements. DHCS awarded $348 million of PATH CITED funds to ECM and Community Supports providers in 2023. Based on the currently available data, however, it is unclear the extent to which these direct grants to providers have led to an increase in the utilization rate within the counties they where they were awarded.
Issues for Legislative Consideration
Utilization of ECM and Community Supports Benefits Have Grown, but There Is an Opportunity for Further Increases. Our analysis of ECM and Community Supports implementation through the first half of the demonstration highlights that while utilization of the benefit may be lower than anticipated, it has grown and may continue to grow as MCPs, providers, and MCP members gain more experience with the benefits. The Legislature will need more information from both DHCS and MCPs to more fully assess whether utilization of the ECM and Community Supports benefits are meeting its expectations, whether utilization will continue to increase, and what possible future state costs could be. DHCS has already indicated it is looking to expand the information available in the quarterly implementation report, and the Legislature could work with the department to ensure that the information provided is sufficient to allow for a robust evaluation of program implementation. While some variation in utilization across counties and MCPs is to be expected, more information is needed to assess what portion of the variation is due to MCPs’ implementation of the benefits. There will also be an evaluation of the PATH initiative to determine whether it expanded ECM and Community Supports provider networks and increased benefit utilization. Some of the key questions the Legislature may wish to have answered by the administration at budget hearings are:
- How many MCP members are potentially eligible for ECM in each MCP and county?
- What Community Supports services do MCPs plan to offer? Why these particular services?
- What is the capacity of plans’ current provider networks to provide ECM and Community Supports services? How can the state facilitate capacity that meets the demand for ECM and Community Supports services?
- What barriers do plans face to increasing access to ECM and Community Supports services?
- What barriers do providers face to contracting with plans to provide ECM and Community Supports services?
More Information Is Needed to Assess Cost‑Effectiveness and Improvements in Health Outcomes. Increasing utilization of the ECM and Community Supports benefit may be an immediate goal of the Legislature, but additional analyses will be needed to determine whether the benefits meet the goals outlined in the program. Based on the evaluations of the WPC and HHP pilot demonstrations, there appears to be some evidence that the ECM benefit may lower costs and improve health outcomes for the state’s high‑cost, high‑need population of Medi‑Cal members. While the terms of the CalAIM waiver require some evaluation of cost‑effectiveness and health outcomes, the Legislature will want to ensure that systems are in place to allow for a robust evaluation of the program’s impacts to the state and MCPs. For example, the Legislature, could consider directing DHCS to conduct an evaluation of the ECM benefit as implemented under CalAIM (even though the waiver does not require this). In the case of Community Supports, an interim evaluation of the benefit is forthcoming from DHCS. That evaluation will assess the cost‑effectiveness of the benefit as well as its impact on the health outcomes of participants. In addition, the Legislature may wish to direct ongoing evaluations to determine whether ECM and Community Supports result in net savings to the state and/or improved health outcomes to beneficiaries. This information would be particularly helpful as the state considers renewing the waiver next year. In the meantime, some of the key questions the Legislature may wish to have answered by the administration at budget hearings are:
- How does DHCS plan to evaluate—on an ongoing basis—the cost‑effectiveness and impacts on health outcomes of the ECM and Community Supports benefits outside of the evaluations required in waivers? What data does it plan to collect, and what reporting from MCPs and providers may it require, to enable the required evaluation under the waiver as well as any ongoing evaluations?
- Does DHCS anticipate renewing the CalAIM waiver? How could the results of the Community Supports interim evaluation impact the CalAIM waiver renewal?
