LAO Contacts
Corrected 2/20/20: Corrected to remove Alameda County from the list counties participating in the Coordinated Care Initiative.
February 14, 2020
The 2020‑21 Budget:
Analysis of the Medi-Cal Budget
- Introduction
- Background
- Overview of the Governor’s Budget
- Medicaid Fiscal Accountability Regulation
- Update on Medi‑Cal Pharmacy Services
- Full‑Scope Expansion for Seniors Regardless of Immigration Status
- SNF Rate Reform
- County Administration
- Proposal to End Dental Managed Care in the Two Pilot Counties
- Summary of Recommendations
Executive Summary
Overall Medi‑Cal Budget Picture. The Governor’s budget proposes $25.9 billion General Fund ($103.5 billion total funds) in 2020‑21, an increase of $2.9 billion (12.4 percent) over estimated 2019‑20 levels. This increase reflects both a number of workload budget adjustments that increase General Fund costs along with new funding to support several policy proposals. Notably, the Governor proposes $348 million General Fund ($695 million total funds) to implement the provisions of a broad set of Medi‑Cal reform proposals collectively referred to as “Medi‑Cal Healthier California for All.” We do not assess these reform proposals in this report, but will do so in a separate forthcoming report.
Administration Recently Submitted a Modified Managed Care Organization (MCO) Tax Proposal for Federal Consideration. For a number of years, the state has imposed a tax on MCOs. Revenues from the MCO tax result in a significant annual General Fund benefit—most recently, nearly $1.3 billion. The MCO tax expired at the end of 2018‑19 and the Legislature reauthorized a new MCO tax in 2019. Because the MCO tax would increase federal Medicaid funding, it requires federal approval. In late January 2020, the federal government rejected the state’s original MCO tax proposal. In early February 2020, the administration—using authority in the MCO tax’s reauthorizing legislation—modified the MCO tax and submitted a new proposal to the federal government. The modified MCO tax proposal would generate a smaller annual General Fund benefit ($1.3 billion to $1.7 billion) than the original proposal (around $2 billion) and have different impacts on MCOs’ tax liability. Federal approval of the modified MCO tax remains uncertain. (We note that as the Governor’s budget does not assume the receipt of revenues from the reauthorized tax until 2021‑22, the fiscal impact of the ultimate federal decision on the state’s proposal will not affect the Governor’s budget structure until 2021‑22.)
Draft Federal Regulation Could Have Significant Fiscal Effects for Medi‑Cal. In October 2019, the federal government released draft regulations related to financing and oversight in the Medicaid program. The draft rule, if implemented in its current or similar form, would require significant changes to major Medi‑Cal financing mechanisms, possibly resulting in several billion dollars of higher General Fund costs. (The modified MCO tax discussed earlier, however, could be approved under existing federal rules.) The ultimate impact of the proposed regulations is highly uncertain and depends on what provisions are in the final rule and how the federal government elects to implement them. However, given the potential for a significant fiscal impact on Medi‑Cal financing, we recommend that the Legislature approach proposals to significantly increase ongoing General Fund expenditures in the 2020‑21 budget with caution.
Governor’s Budget Includes Various Proposals Intended to Result in Pharmacy Savings. This report analyzes the Governor’s pharmacy‑related proposals that implicate Medi‑Cal and the Department of Health Care Services (DHCS), including (1) changes to facilitate the transition of Medi‑Cal pharmacy services from a managed care to a fee‑for‑service (FFS) benefit, which include proposed supplemental payments for clinics to mitigate associated financial losses, and (2) budget‑related legislation authorizing DHCS to collect rebates on drugs not paid for through Medi‑Cal. First, we find that the Governor’s savings estimate for the transition of Medi‑Cal pharmacy services to an FFS benefit likely is overstated. We recommend that the Legislature enact report requirements to ensure that this major policy change is achieving its objective of generating state savings. Additionally, we question whether the Governor’s proposed supplemental payments for clinics serve a public purpose in the long run, and recommend either making the payments temporary or, if made ongoing as proposed, tying them to quality and/or access improvements.
Governor Proposes Expanding Comprehensive Coverage for Income‑Eligible Seniors, Regardless of Immigration Status. Historically, income‑eligible undocumented immigrants only qualified for “restricted‑scope” Medi‑Cal coverage, which covers emergency‑ and pregnancy‑related health care services. Over the last several years, the Legislature has expanded comprehensive “full‑scope” Medi‑Cal coverage to undocumented children ages 0 through 18 and adults ages 19 through 25. The Governor proposes to expand full‑scope Medi‑Cal coverage to income‑eligible undocumented seniors ages 65 and older beginning in January 2021. The Governor projects $64 million will be needed to fund this half‑year expansion in 2020‑21. We project that this expansion will cost around $250 million on an ongoing basis, with this funding split between Medi‑Cal and the In‑Home Supportive Services program.
Proposed Skilled Nursing Facilities (SNF) Rate Reform Has Promise, But Many Questions Remain. The state’s current system for setting reimbursement rates for SNF sunsets in August 2020. The Governor proposes to reauthorize the rate‑setting system with several changes. Overall, these changes intend to increase the role of SNF quality in setting rates. The Governor also proposes to extend a quality assurance fee paid by SNF that offsets the General Fund costs of SNF reimbursement. We find that, in concept, better integrating quality incentives with rates could strengthen incentives for SNF to improve quality. However, many questions remain about the proposal, such as how the proposed rate system would function in the managed care environment. (The Governor has separately proposed transitioning SNF care to the managed care delivery system statewide.) We recommend that the Legislature withhold action on this proposal until more information is provided. Should the Legislature adopt the Governor’s proposal, we recommend requiring an evaluation of the new rate structure’s impact on SNF quality.
Increased Oversight of County Medi‑Cal Administration Is Warranted. Implementation of the Patient Protection and Affordable Care Act (ACA) was disruptive to county Medi‑Cal administration. Federal and state audits have identified deficiencies in county administration and the state’s oversight of these activities during and following ACA implementation. Further, the analytical basis for the state’s approach to budgeting for county administrative activities has significantly eroded. The Governor proposes to provide a cost‑of‑living adjustment for county administration funding (consistent with recent practice) with no other changes to the state’s budgeting methodology. The Governor further proposes to reinstate and build on county oversight processes that previously were suspended. We recommend that the Legislature require the administration to provide an update on county performance and efforts to improve performance prior to approving the Governor’s proposals. We further recommend that the Legislature adopt a plan for revising the budgeting methodology for county Medi‑Cal administration.
Proposal to End Dental Managed Care. For over 25 years, the state has operated a dental managed care pilot program in Sacramento and Los Angeles Counties whereby Medi‑Cal dental services are accessed through specialty dental managed care plans rather the typical Medi‑Cal dental FFS delivery system. The Governor proposes to end the dental managed care pilot program and transition Medi‑Cal dental services to FFS in the two pilot counties. In our assessment, dental managed care has not achieved its objectives of achieving savings while ensuring access and quality. Accordingly, we recommend approval of the Governor’s proposal assuming no information is obtained during the budget process that shows clear improvement in the dental managed care plan performance.
Introduction
Report Provides Assessment of Overall Medi‑Cal Budget Proposal… With proposed General Fund expenditures of nearly $26 billion, Medi‑Cal is one of the largest items in the state’s budget. This report provides a broad overview of the major spending changes reflected in the Governor’s proposed Medi‑Cal budget, as well as analysis and recommendations on several proposals for legislative consideration.
…But Does Not Assess Medi‑Cal Healthier California for All. This report does not provide analysis and recommendations on the Governor’s proposed broad Medi‑Cal reform effort, referred to as “Medi‑Cal Healthier California for All” (MHCA). We will provide our comments on that reform proposal in a separate forthcoming report.
Layout of This Report. This report begins with some high‑level background on the Medi‑Cal program, followed by an overview of the major drivers of year‑over‑year spending changes in the Governor’s budget. We also discuss the administration’s recent submittal (late January 2020) of a modified managed care organization (MCO) tax proposal. Following this section, we provide analysis and recommendations on a series of key issues:
- Recently proposed draft federal regulations referred to as the “Medicaid Fiscal Accountability Regulation.”
- Proposals related to the Medi‑Cal pharmacy services benefit.
- The Governor’s proposal to expand comprehensive Medi‑Cal coverage to otherwise eligible seniors regardless of immigration status.
- Proposed changes to rate‑setting for skilled nursing facilities (SNFs).
- Issues related to county administration of eligibility and enrollment functions in Medi‑Cal.
- The Governor’s proposal to end dental managed care in the current two pilot counties and instead provide dental care as a fee‑for‑service (FFS) benefit statewide.
We conclude this report with a summary table of our recommendations.
Background
Medi‑Cal, the state’s Medicaid program, is administered by the Department of Health Care Services (DHCS) and provides health care coverage to almost 13 million of the state’s low‑income residents. Coverage is cost‑free for most Medi‑Cal enrollees. Instead, Medi‑Cal costs generally are shared between the federal, state, and local (county) governments.
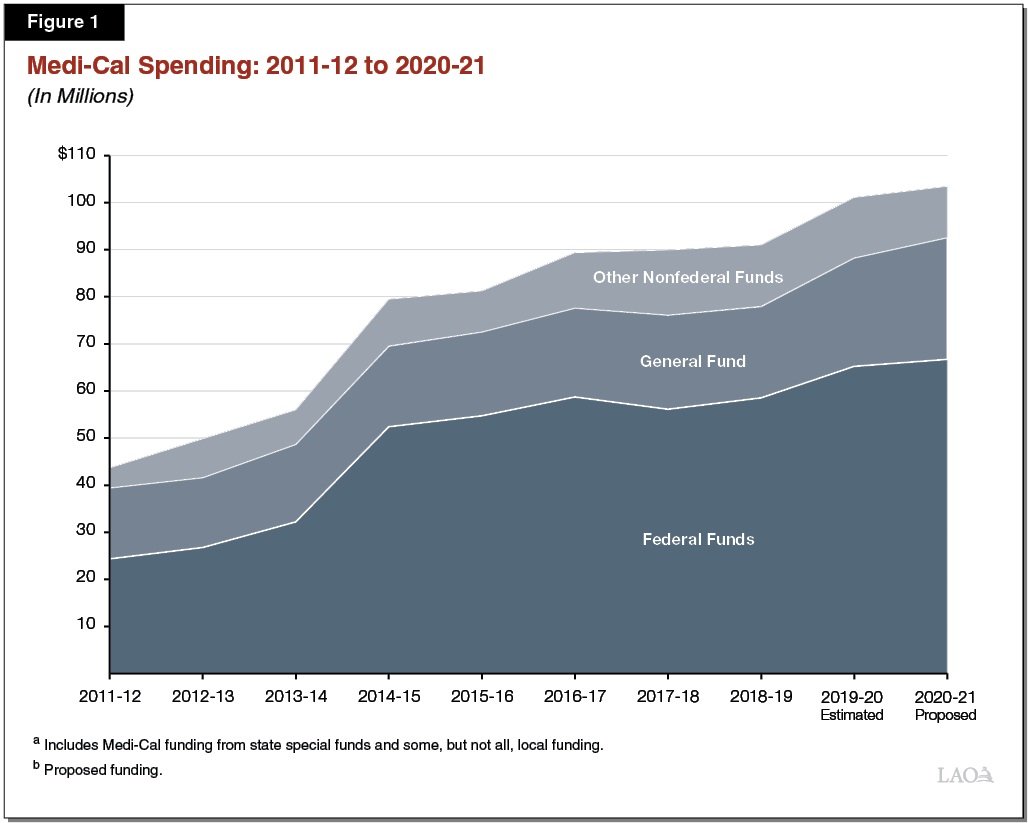
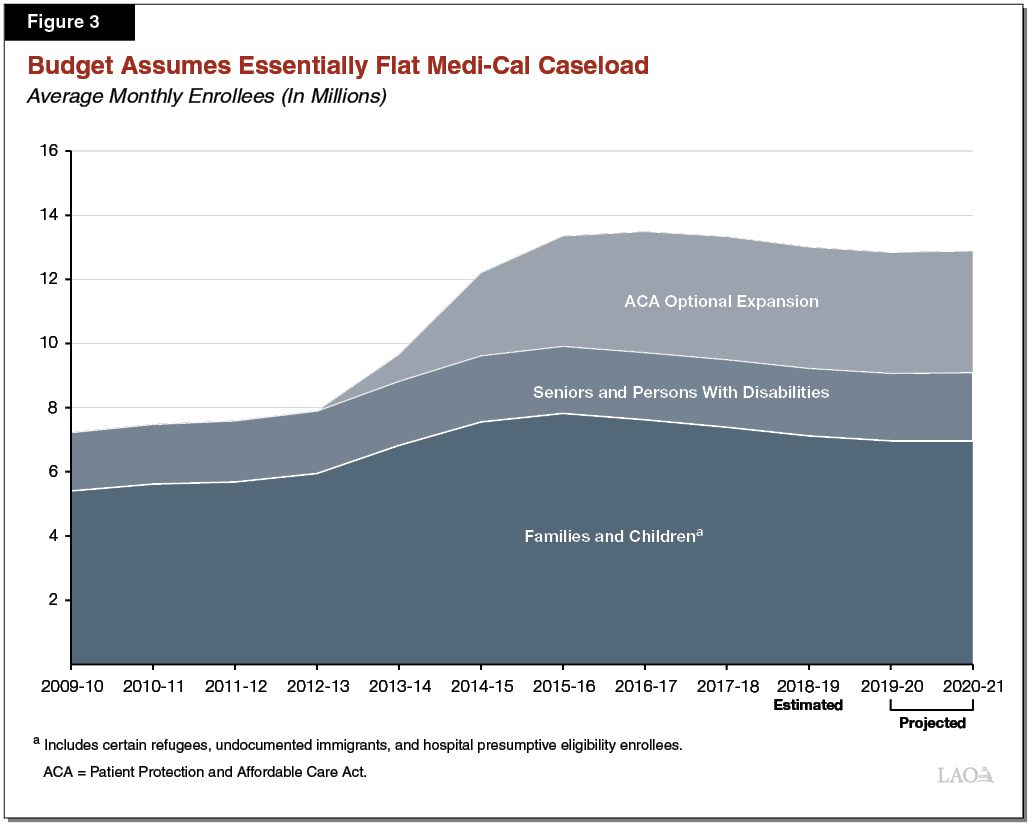
Medi‑Cal Has Grown Significantly Under the Patient Protection and Affordable Care Act (ACA). Before 2014, Medi‑Cal eligibility mainly was restricted to low‑income families with children, seniors, persons with disabilities, and pregnant women. As allowed under the ACA, in 2014, the state expanded Medi‑Cal eligibility to include additional low‑income populations—primarily childless adults who did not previously qualify for the program. This eligibility expansion sometimes is referred to as the “ACA optional expansion.” Medi‑Cal has grown significantly both in terms of caseload and spending as a result of the ACA optional expansion and the other changes under the ACA to encourage health care coverage. Figure 1 shows the growth in Medi‑Cal spending over the last decade. Figure 3, found later in this report, shows the significant increase in Medi‑Cal caseload from nearly 8 million enrollees to over 13 million enrollees in the years following implementation of the ACA, with the caseload leveling off recently.
Federal Share of Cost Varies, Primarily by Eligibility Group. The costs of state Medicaid programs generally are shared between the federal government and states based on a set formula. The percentage of Medicaid costs paid by the federal government is known as the federal medical assistance percentage (FMAP).
For most low‑income families and children, seniors, persons with disabilities, and pregnant women, California generally receives a 50 percent FMAP—meaning the federal government pays half of Medi‑Cal costs for these populations. For the subset of children in families with higher incomes that qualify for Medi‑Cal as part of the Children’s Health Insurance Program (CHIP), the federal government pays 76.5 percent of the costs and the state pays 23.5 percent. (The state share is scheduled to ramp up to the historical cost share of 35 percent over the coming years.) Under the ACA, the federal government paid 100 percent of the costs of providing health care services to the ACA optional expansion population from 2014 through 2016. Beginning in 2017, the federal cost share decreased to 95 percent and phases down further to 90 percent in 2020 and thereafter.
Delivery Systems. There are two main Medi‑Cal systems for the delivery of medical services: FFS and managed care. In the FFS system, a health care provider receives an individual payment from DHCS for each medical service delivered to a beneficiary. Beneficiaries in Medi‑Cal FFS generally may obtain services from any provider who has agreed to accept Medi‑Cal FFS payments. In managed care, DHCS contracts with managed care plans to provide health care coverage for Medi‑Cal beneficiaries. Managed care enrollees may obtain services from providers who accept payments from the managed care plan, also known as a plan’s “provider network.” The plans are reimbursed on a “capitated” basis with a predetermined amount per person per month, regardless of the number of services an individual receives. Medi‑Cal managed care plans provide enrollees with most Medi‑Cal covered health care services—including hospital, physician, and pharmacy services—and are responsible for ensuring enrollees are able to access covered health care services in a timely manner. Managed care enrollment is mandatory for most Medi‑Cal beneficiaries, meaning these beneficiaries must access most of their Medi‑Cal benefits through the managed care delivery system. FFS enrollment largely consists of newly enrolled beneficiaries who will soon enroll in a managed care plan and certain seniors and persons with disabilities. In 2019‑20, more than 80 percent of Medi‑Cal beneficiaries are estimated to be enrolled in managed care.
Overview of the Governor’s Budget
Current‑Year Adjustments
Estimated General Fund Spending Down $92 Million in 2019‑20. The Governor’s budget projects that Medi‑Cal spending will be $92 million lower (0.4 percent) in 2019‑20 relative to what was assumed in the 2019‑20 Budget Act. This is a small current‑year adjustment relative to previous years. The downward adjustment primarily reflects (1) savings from reduced expected enrollment in the program and (2) a number of other, primarily technical adjustments that largely offset one another.
Budget‑Year Adjustments and Proposals
Under the Governor’s proposed budget, General Fund spending in Medi‑Cal would grow from $23 billion in 2019‑20 to $25.9 billion in 2020‑21—a $2.9 billion, or 12.4 percent, increase in year‑over‑year spending. Figure 2 summarizes the major factors responsible for the proposed growth in General Fund spending in Medi‑Cal, which includes both workload budget adjustments and new policy proposals.
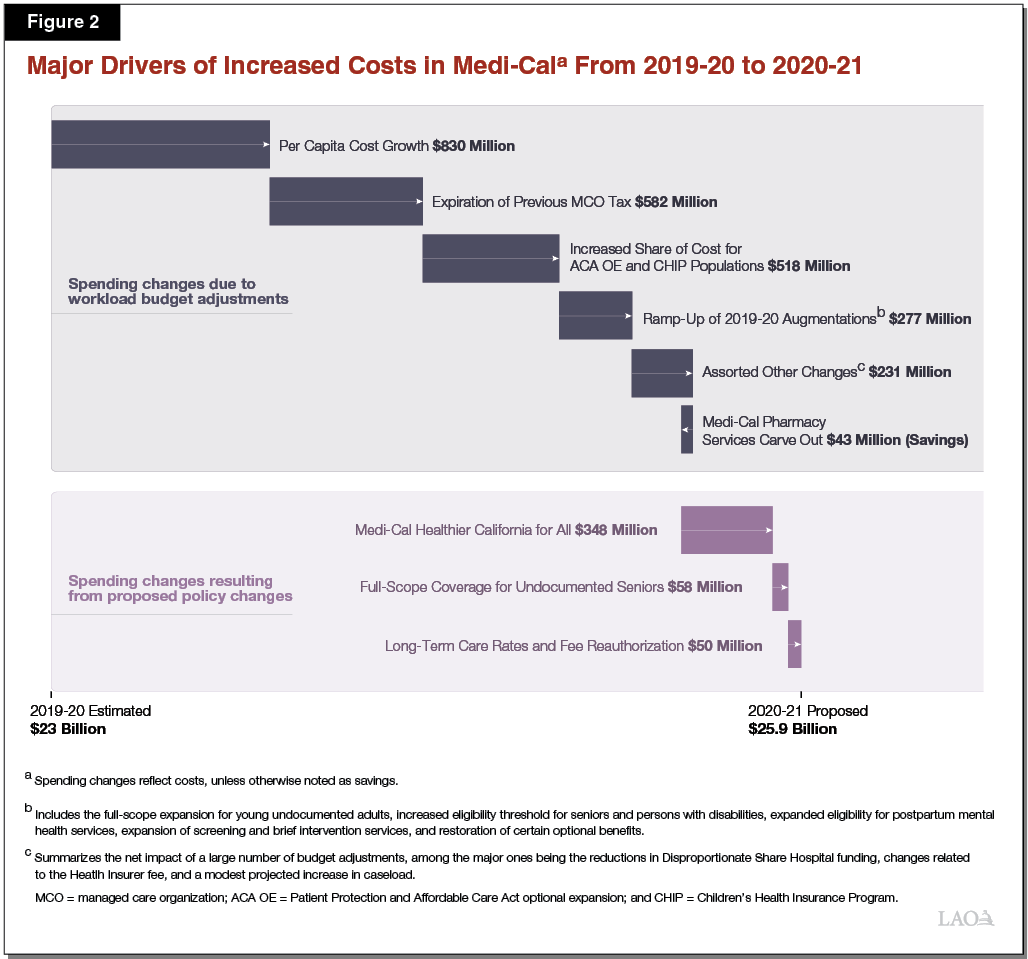
Workload Budget Adjustments. Most of this change in General Fund spending from 2019‑20 to 2020‑21 is due to workload budget adjustments. We describe several major adjustments below.
- Governor’s Budget Cautiously Assumes Caseload Essentially Will Be Flat Going Into 2020‑21. As shown in Figure 3, the Governor’s budget projects that the Medi‑Cal caseload will remain essentially flat in 2020‑21, growing only by 0.4 percent to an average of 12,880,440 enrollees per month. This assumption results in higher General Fund costs in the low tens of millions of dollars relative to 2019‑20. In our view, the Governor’s Medi‑Cal caseload estimates are cautious as we project that the caseload will continue to decline slowly, provided that the economy continues to expand. (In recent years, caseload declined by around 1 percent to 2 percent per year on average.) The Governor will provide updated caseload estimates in May, at which time we will reassess the reasonableness of the administration’s Medi‑Cal caseload assumptions.
- Per Capita Cost Growth. We estimate that per capita cost growth accounts for $830 million of the increase in spending relative to 2019‑20.
- MCO Tax. The Medi‑Cal budget reflects a $582 million increase relative to 2019‑20, due to the expiration of the previous MCO tax and the Governor’s budget assumption that revenues from the MCO tax recently reauthorized by the Legislature would not materialize until 2021‑22.
- Scheduled Reductions in Federal Share of Costs. We estimate that the Medi‑Cal budget reflects a $518 million increase in spending relative to 2019‑20 due to scheduled changes in the federal share of costs for the ACA optional expansion and CHIP populations.
- Ramp‑Up of 2019‑20 Augmentations. The Medi‑Cal budget reflects a $277 million increase in spending relative to 2019‑20 due to continued implementation of 2019‑20 augmentations. These augmentations include (1) the expansion of full‑scope Medi‑Cal to otherwise eligible young adults regardless of immigration status, (2) an increased income eligibility threshold for certain seniors and persons with disabilities, (3) expanded eligibility for postpartum mental health services, (4) expansion of screening and intervention for substance use disorder services, and (5) the restoration of certain optional Medi‑Cal benefits.
- “Disproportionate Share Hospital” Reduction. The Medi‑Cal budget reflects an $83 million reduction in spending on payments to private disproportionate share hospitals, which serve large numbers of low‑income or uninsured populations. This state reduction is triggered by a scheduled reduction in federal funding for payments the state largely directs to public disproportionate share hospitals. (Congress has repeatedly delayed the scheduled federal reduction and may do so again. If this happens, the General Fund savings identified in the Governor’s budget on payments to private disproportionate share hospitals may be reduced or may not materialize at all.)
New Policy Proposals. Nearly $490 million of the increase in General Fund spending is attributable to new discretionary policy proposals that are included in the Governor’s budget.
- MHCA. The administration’s recently introduced MHCA proposal intends to significantly overhaul the state’s Medi‑Cal system, and introduces new benefits intended to provide more comprehensive care to patients with more complex health needs. The Medi‑Cal budget proposes spending $348 million from the General Fund ($695 million total funds) in 2020‑21 to implement MHCA. Under the Governor’s proposal, spending would double to $695 million General Fund ($1.4 billion total funds) in 2021‑22 and 2022‑23. Beginning in 2023‑24, ongoing annual costs would be $395 million General Fund ($790 million total funds).
- Expansion of Comprehensive (“Full‑Scope”) Medi‑Cal Coverage to Seniors Regardless of Immigration Status. The administration proposes extending comprehensive Medi‑Cal coverage to income‑eligible seniors aged 65 and older regardless of immigration status. The Medi‑Cal budget provides $58 million in 2020‑21 to implement this proposal for a half year. On an annual basis, we project Medi‑Cal General Fund costs for the expansion to be around $110 million.
- SNF Rate Reform. The administration proposes reforming the way in which SNF rates are set. In recent years, SNF rates have received an annual increase and the Governor’s proposal would continue this practice. However the Governor additionally proposes providing an additional midyear rate increase in 2020‑21, related to transitioning SNF rate setting from a state fiscal‑year basis to a calendar‑year basis. Budget documents released on January 10, 2020 indicate that the General Fund cost of this midyear increase will be around $50 million in 2020‑21. The ongoing costs of this midyear adjustment would be roughly double this amount.
- Supplemental Payment Pool for Clinics to Mitigate Loss in Earnings Due to Changes to Medi‑Cal Pharmacy Services. To mitigate the loss in earnings for clinics due to changes to Medi‑Cal pharmacy services, the Governor proposes half‑year funding of $26 million General Fund ($53 million total funds) to create a new supplemental payment program.
Administration Recently Resubmitted a Modified MCO Tax Proposal
Background. For a number of years, the state has imposed a tax on MCOs’ Medi‑Cal and commercial lines of business. This tax historically raised significant special fund revenues ($2.6 billion in 2018‑19), which generate a General Fund benefit (most recently, nearly $1.3 billion in 2018‑19) by offsetting a portion of General Fund expenditures in Medi‑Cal. Following the expiration of the most recent MCO tax, which was in place from 2016‑17 through 2018‑19, the Legislature reauthorized the MCO tax last year under a somewhat modified structure from the previous tax. The reauthorized MCO tax would generate a General Fund benefit of $1 billion to $2 billion annually from 2019‑20 to 2023‑24. Because the reauthorized MCO tax would increase federal Medicaid funding, it requires federal approval. For more information on the reauthorized MCO tax, see our Budget and Policy Post: The 2019‑20 Budget: California Spending Plan—Health and Human Services.
Governor’s Budget Assumes a Delayed Implementation of the Reauthorized MCO Tax. Due to uncertainty regarding the timing of federal approval of the reauthorized MCO tax, the Governor’s budget assumed a delay in when the General Fund benefit from the reauthorized MCO tax would materialize. Accordingly, the Governor’s budget assumes the General Fund benefit from the MCO tax would materialize in 2021‑22 rather than in either 2019‑20 or 2020‑21.
Federal Government Rejected the State’s Initial Proposal for a Reauthorized MCO Tax. In late January 2020, after the release of the Governor’s budget, the federal government notified the state of its decision to reject the state’s proposal for a reauthorized MCO tax. The federal government rejected the reauthorized MCO tax proposal under existing federal rules. Based on our understanding, the federal government rejected the state’s proposal, at least in part, due to the reauthorized tax not imposing any liability on MCOs that do not have Medi‑Cal membership, thereby—in the federal government’s view—violating the no‑hold harmless requirement in existing federal law.
Administration Has Submitted a Modified MCO Tax Proposal for the Federal Government to Consider. In the reauthorizing legislation for the MCO tax, the Legislature gave the administration authority to modify the structure of the MCO tax in order to gain federal approval, provided that the modifications do not significantly increase the total tax amounts projected to be collected under the tax. The administration has used this authority and, in early February, resubmitted a modified MCO tax proposal to the federal government for consideration.
To gain federal approval, the administration has modified the MCO tax proposal in a way that increases the net tax liability on a number of MCOs, specifically by lowering the enrollee threshold for taxation on non‑Medi‑Cal membership. In effect, this would increase the net liability on four MCOs that have no Medi‑Cal membership. By imposing a net liability on MCOs without Medi‑Cal membership, the state’s modified MCO tax proposal is intended to address the federal government’s principal objection to the structure of the recently rejected, original proposal.
Figure 4 compares the structure of the original and modified MCO tax structures. Figure 5 compares the fiscal impact in the first year of implementation. The net General Fund benefit of the modified MCO tax would be lower than that of the rejected tax. Rather than generating a General Fund benefit of up to around $2 billion on an annual basis, the modified MCO tax would generate a $1.3 billion to $1.7 billion General Fund benefit on annual basis. The lower benefit is largely due to effectively eliminating the tax on MCOs’ first 675,000 Medi‑Cal enrollees. Moreover, some MCOs will face higher net tax liability under the modified proposal, while others will face lower net tax liability. As with the original proposal, the modified proposal would be in place for 3.5 years.
Federal Decision, if Maintained, Significantly Raises the Amount of General Fund Needed for Medi‑Cal Beyond 2020‑21. If the state ultimately does not obtain federal approval on the modified MCO tax proposal, an additional $1 billion to $2 billion of General Fund would be needed annually to fully fund the Medi‑Cal program starting in 2021‑22. This amount is relative to the multiyear assumptions included in the Governor’s budget.
Figure 4
Comparing the Tax Rates of the Original and Modified MCO Tax Proposals
|
Member Monthsa |
Tax Rate Per Member Month |
|
|
Original Proposalb |
Modified Proposalc |
|
|
Medi‑Cal Enrollees |
||
|
1‑675,000 |
$40 |
— |
|
675,001‑4,000,000 |
40 |
$40 |
|
4,000,001 and above |
— |
— |
|
Commercial Enrollees |
||
|
1‑675,000 |
— |
— |
|
675,001‑4,000,000 |
— |
$1 |
|
4,000,001 to 8,000,000 |
$1 |
— |
|
8,000,001 and above |
— |
— |
|
aA member month is defined as one member being enrolled for one month in an MCO. bOriginal proposal refers to the MCO tax as reauthorized and proposed to the federal government for consideration in 2019. cModified proposal refers to the MCO tax as modified by the administration and proposed to the federal government for consideration in 2020. |
||
|
MCO = managed care organization. |
||
Figure 5
Comparing the Fiscal Impacts of the Original and Modified MCO Tax Proposals
LAO Estimates for First Full Year of Implementation (In Millions)
|
State Impact |
Original Proposala |
Modified Proposalb |
Difference |
|
Total MCO tax revenue |
$2,631 |
$2,063 |
‑$568 |
|
General Fund cost of Medi‑Cal reimbursement to MCOs |
‑915 |
‑714 |
201 |
|
Net General Fund Benefit |
$1,716 |
$1,349 |
‑$367 |
|
Health Insurance Industry Impact |
|||
|
MCO tax liability |
$2,631 |
$2,063 |
‑$568 |
|
Medi‑Cal reimbursement to MCOs |
‑2,614 |
‑2,040 |
574 |
|
Net Health Insurance Industry Liability |
$17 |
$23 |
$6 |
|
aOriginal proposal refers to the MCO tax as reauthorized and proposed to the federal government for consideration in 2019. bModified proposal refers to the MCO tax as modified by the administration and proposed to the federal government for consideration in 2020. |
|||
|
MCO = managed care organization. |
|||
Extends Potential Suspensions to 2023‑24
To prevent a potential General Fund operating deficit from arising in the years after 2019‑20, the 2019‑20 Budget Act adopted provisional suspension language that applies to a number of recent, mostly health and human services augmentations. Figure 6 lists the four Medi‑Cal augmentations subject to the suspension language. The 2019‑20 Budget Act’s provisional language suspends all of the augmentations subject to the language as of January 1, 2022 unless the Department of Finance determines in May 2021 that annual General Fund operating surpluses could accommodate all the augmentations over the next two fiscal years. The Governor’s 2020‑21 budget proposes to extend the effective date of the suspensions for one‑and‑a‑half years to July 1, 2023. Accordingly, the four Medi‑Cal augmentations listed in Figure 6 would be suspended starting in 2023‑24 unless the Department of Finance determines that there is sufficient General Fund to support all the augmentations subject to the suspension language in 2023‑24.
Figure 6
Medi‑Cal Augmentations Subject to
Potential Suspension
General Funds (In Millions)
|
Proposition 56 Medi‑Cal provider payment increasesa |
$819 |
|
Extension of Medi‑Cal coverage for postpartum mental health |
46 |
|
Medi‑Cal optional benefits restoration |
34 |
|
Expansion of screening and intervention in Medi‑Cal to drugs other than alcohol |
3 |
|
Total |
$902 |
|
aThe Proposition 56 funding for Medi‑Cal no longer supporting provider payment increases would be used to offset General Fund spending on cost growth in Medi‑Cal. |
|
Medicaid Fiscal Accountability Regulation
In October 2019, the federal government released draft regulations related to financing and oversight in the Medicaid program. These rules, if implemented in their current or a similar form, would require significant changes to major Medi‑Cal financing mechanisms, possibly resulting in several billion dollars of higher General Fund costs. These rules also would dramatically increase the amount and types of information the state would be required to report to the federal government. In this section, we provide background on how the nonfederal share of Medi‑Cal costs is financed and the major provisions of the proposed regulations. The provisions of the draft federal regulations are likely to change before being finalized, so the ultimate impact on the state is highly uncertain.
Medi‑Cal Is Partly Financed From a Variety of Non‑General Fund Sources
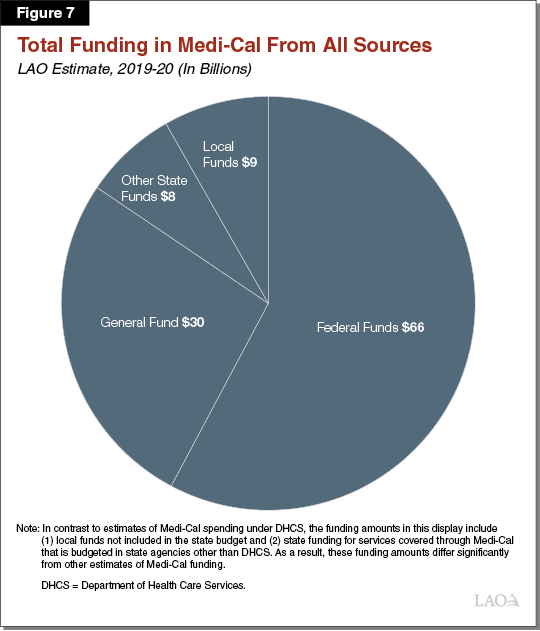
Figure 7 displays total funding for Medi‑Cal in 2019‑20 and 2020‑21 under the Governor’s proposal. As shown in the figure, the state uses a variety of non‑General Fund sources to finance the nonfederal share of Medi‑Cal, including local funds, health care‑related taxes, and state special funds. We describe these nonfederal funding sources below.
Local Funds
Some Local Governments Operate Health Facilities That Serve Medi‑Cal Enrollees. Some local government entities in the state—including some counties, cities, and special districts—operate health care facilities, such as hospitals and clinics. These government‑operated facilities are part of the state’s health care “safety net,” a term which is sometimes used to refer to health care providers that provide care regardless of an individual’s health insurance coverage status or ability to pay for care. Medi‑Cal enrollees and the uninsured typically make up a large share of these providers’ patients. Local governments that operate health facilities receive payment through the Medi‑Cal program for the services that they provide to Medi‑Cal enrollees.
Local Governments Also Contribute Toward the Nonfederal Share of Medi‑Cal Costs. In addition to providing health care services to Medi‑Cal enrollees, local governments also contribute toward financing the nonfederal share of cost in Medi‑Cal. There are two mechanisms established in federal law through which local governments contribute to financing Medi‑Cal:
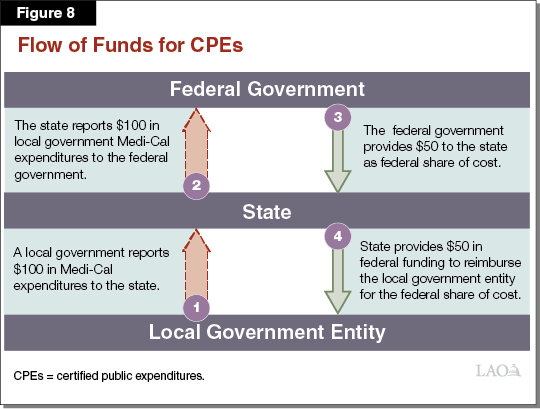
- Certified Public Expenditures (CPEs). Under the first mechanism, a local government incurs costs providing covered health care services to Medi‑Cal enrollees. The local government certifies to the state that expenditures were made and the state then makes a claim to the federal government to receive funding to cover the federal share of the expenditures. This federal funding is then used to reimburse the local entity for the federal share of the expenditure. As described earlier, the portion of Medi‑Cal expenditures covered by the federal government varies depending on the population being served. Figure 8 provides an example of how funds would flow through this CPE process assuming an FMAP of 50 percent. We estimate that CPEs account for around $3.1 billion in Medi‑Cal funding in 2019‑20.
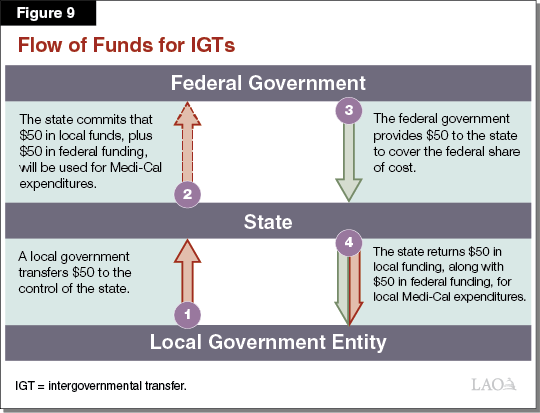
- Intergovernmental Transfers (IGTs). Under the second mechanism, local governments transfer funding to the control of the state, which then commits to the federal government that the funding will be used in the future for Medi‑Cal expenditures. The federal government provides the state funding to cover the federal share of cost of the future expenditures and the state then provides both the local funding and the federal funding to the local government for Medi‑Cal expenditures. Under current practice and consistent with federal approvals to date, funding that local governments provide as an IGT can come from various sources, such as revenue the local government entity receives from providing health care services and local tax revenues. Figure 9 provides an example of how funds would flow through the IGT process assuming an FMAP of 50 percent. We estimate that IGTs account for about $4.6 billion in Medi‑Cal funding in 2019‑20.
Funds From Health Care‑Related Taxes
Federal Government Currently Regulates Health Care‑Related Taxes. Many states levy licensing fees, assessments, or other mandatory payments on the provision of health care services or products. These are referred to as “health care‑related taxes.” Given its significant role in funding health care, the federal government has existing rules that regulate states’ health care‑related taxes to the extent that these are levied to draw down federal funds. The rules apply, for example, to taxes on direct health care services (such as hospital inpatient stays) as well as payers of health care services (such as health insurer revenue or enrollment).
The rules are in place to prevent states from imposing too disproportionate a burden on federal Medicaid funds to pay the tax. Therefore, to receive federal approval, a state must prove to the federal government that the burden of paying a health care‑related tax does not fall too disproportionately on Medicaid as opposed to non‑Medicaid services. Specifically, health care‑related taxes must pass a complex statistical test that determines whether the tax falls too disproportionality on federal Medicaid funds. To further ensure that the tax liability is distributed broadly among Medicaid and non‑Medicaid services, a state cannot hold payers of the health care‑related tax harmless by providing its payers direct or indirect payments to offset the tax. While a state may implement a health care‑related tax that violates federal rules, the federal government reduces funding for the state’s Medicaid program in proportion to the revenues raised by an impermissible tax, making imposition of such taxes highly unappealing.
Medi‑Cal Relies on Revenues From Several Health Care‑Related Taxes. California has—or until recently has had in place—several health care‑related taxes that, together, generate significant revenues that help finance the Medi‑Cal program and often serve to offset what would otherwise be General Fund costs. We describe these taxes below.
- MCO Tax. As previously discussed, in 2019, the state proposed for federal approval a reauthorized MCO tax that would generate a General Fund benefit of up to roughly $2 billion annually. While no revenues from the MCO tax are assumed in the Governor’s budget to offset General Fund spending in Medi‑Cal in either 2019‑20 or 2020‑21, the administration, in the January budget, assumes such revenues would offset General Fund Medi‑Cal spending starting in 2021‑22. As also noted, in early February of this year, the state submitted a modified MCO tax proposal following the federal government’s late‑January decision to reject the California’s original MCO tax proposal on the basis of current federal rules related to health care‑related taxes.
- Hospital Quality Assurance Fee (QAF). Under the hospital QAF, the state assesses a tax on private hospitals based on the amount of care they provide to Medi‑Cal enrollees and other populations (measured in terms of bed days), totaling a projected $3.5 billion in 2019‑20. Most of the QAF revenues are used to provide supplemental payments to private hospitals and a small amount of grant funding to public hospitals, increasing their total overall reimbursement for services provided to Medi‑Cal enrollees. Another portion of the hospital QAF funding is kept by the state to offset what otherwise would be General Fund costs, a projected $914 million in 2020‑21. The Legislature first established the hospital QAF in 2009. The hospital QAF was later reauthorized by the Legislature several times. In 2018, voters approved Proposition 52, which made permanent the statutory authority for the state to assess the hospital QAF and provide the associated supplemental payments and grant funding. However, the state is required to seek federal approval for adjustments to the QAF and related supplemental payments every few years.
- Other Provider Fees and Taxes. The state has a few other, relatively minor, provider taxes, listed below:
- SNF QAF. The state assesses a fee on SNF bed days that is used to offset the state’s General Fund costs for SNF services in Medi‑Cal. The SNF QAF is projected to raise $505 million in 2019‑20.
- Ground Emergency Medical Transportation (GEMT) QAF. The state assesses a fee on GEMT that is used to raise reimbursement levels for GEMT providers and offset what otherwise would be General Fund costs in Medi‑Cal. The GEMT QAF is projected to raise around $200 million in 2019‑20.
- Intermediate Care Facility (ICF) QAF. The state assesses a fee on the gross receipts of certain ICFs that is used to offset state costs for ICF services. The ICF QAF is projected to raise $35 million in 2019‑20.
Other Special Funds
In addition to local funds and revenues from health care‑related taxes, the state relies on a number of other state special funds to finance the nonfederal share of cost in Medi‑Cal. For example, Medi‑Cal’s most significant source of other state special fund revenue is from state taxes on tobacco products, including the approximately $1 billion in Proposition 56 (2016) revenue that supports provider payment increases in Medi‑Cal.
As Proposed, Federal Regulations Would Change Medicaid Financing and Oversight
Below, we describe provisions of the draft federal regulations that would have the greatest impact on Medi‑Cal.
Changes Related to Allowable Sources of Funding
The draft regulations significantly change what the federal government would allow as a source of nonfederal funding for Medi‑Cal.
- Would Limit Use of State Special Funds. The draft regulation specifies that state funding for Medi‑Cal would need to come from the General Fund, which would appear to preclude the possibility of the state using state special funds, such as those that receive tobacco tax revenues, to finance Medi‑Cal.
- Would Limit Permissible Sources of IGTs. The draft regulation also specifies that the source of IGTs would be limited to state and local government tax revenues. This limitation would exclude local governments’ patient care revenue—a very significant source of funding for IGTs under current financing structures.
Changes Specific to Health Care‑Related Taxes
New Proposed Rules Would Prohibit Health Care‑Related Taxes From Placing an Undue Burden on Medicaid. As previously noted, the federal government already has rules that effectively prohibit health care‑related taxes if the tax burden falls too disproportionately on Medicaid as opposed to non‑Medicaid services. Under the proposed federal regulations, the federal government would add additional, nonstatistical tests beyond the existing statistical test to determine whether a health care‑related tax falls too disproportionately on Medicaid services. These additional tests would effectively prohibit health care‑related taxes that place different tax rates on taxpayers based on their levels of Medicaid (versus non‑Medicaid) activity. In addition, the new federal rule would give the federal government significant discretion—beyond the tests—to determine whether a proposed health care‑related tax places an undue burden on Medicaid as opposed to non‑Medicaid services.
Significantly Increases Reporting Requirements
The draft regulations would significantly expand the amount and types of information the state would be required to provide to the federal government. These new reporting requirements could result in significant new state costs.
Requires Provider‑Level Reporting on Supplemental Payments. The state provides supplemental payments (that is, payments on top of base rates that increase overall compensation) to various Medi‑Cal providers, and currently reports information about the aggregate amount of these supplemental payments to the federal government. Under the proposed regulation, the state would be required to provide information on the amount of supplemental payments provided to each individual provider.
Would Require More Frequent Reauthorization of Supplemental Payments. For many of the state’s supplemental payments, the state periodically seeks reauthorization from the federal government to continue the program. For some supplemental payment programs, however, the state is not currently required to seek periodic reauthorization. Under the proposed regulation, the state would be required to seek federal reauthorization every three years for all payments.
Would Require Evaluation of Supplemental Payments. In connection with the periodic reauthorization described above, the state would be required to commit to evaluating the impacts of supplemental payments on quality and access to services. The state generally has not been required to conduct such evaluations in the past.
Allows Temporary “Grandfathering” Period
The draft regulations include a provision allowing states to continue financing structures and supplemental payments that do not comply with the regulation for a period of no more than three years after the regulations are finalized, provided that federal approval was in place before the regulations are finalized. We understand that the regulations could be finalized this summer, but this is uncertain. Notably, the state recently applied for approval of the most recent iterations of the hospital QAF and the MCO tax.
Potential Impacts in Medi‑Cal
State May Be Unable to Continue Various Financing Mechanisms Without Significant Changes. If the draft regulations were finalized in their current or similar form, many of the state’s mechanisms for financing Medi‑Cal with non‑General Fund sources would be at risk of being disallowed. For financing mechanisms that are disallowed, the Legislature would need to make a choice as to whether to replace the non‑General Fund sources with General Fund, restructure the financing mechanism (where feasible) to make it compliant with the regulations (which would likely require either the state or other entities to increase their contribution toward Medi‑Cal costs), or reduce spending in the Medi‑Cal program to account for the lost funding.
Ultimately, the draft federal regulations likely would have different impacts on different Medi‑Cal financing mechanisms. Consequently, the entire amount of funding from local funds and other state funds displayed in Figure 7 is not necessarily at risk. For some financing mechanisms, such as the MCO tax, the provisions of the state’s tax are clearly incompatible with the provisions of the draft rule and being able to continue this financing mechanism in the future is unlikely. In other cases, depending on the contents of the final rule, the state might be able to make relatively modest adjustments to come into compliance with the regulations, mitigating the fiscal impact on the state. Other items, such as the SNF QAF, appear to largely comply with provisions of the draft regulations, so any impact may be limited. At this time, we estimate that the state could face increased annual General Fund costs in the several billions of dollars if the draft regulations were finalized in their current or similar form and the state were to maintain Medi‑Cal funding at current levels.
Ultimate Impact of Proposed Regulations Highly Uncertain. The provisions of the draft regulations would have significant adverse impacts for Medicaid programs in many other states. In light of this, there is a strong possibility that some provisions of the draft regulation could be changed before the regulation is finalized. The ultimate fiscal impact of the regulations on the state will depend on what provisions are in the final rule and how the federal government elects to implement them. Additionally, as noted previously, some financing mechanisms that are ultimately found to be noncompliant with the final regulations may be grandfathered if federal approval is achieved before the rule is finalized. These factors make the ultimate impact of the proposed regulations on the state highly uncertain. However, given the potential for a significant fiscal impact on Medi‑Cal financing, we recommend that the Legislature approach proposals to significantly increase ongoing General Fund expenditures with caution.
Update on Medi‑Cal Pharmacy Services
This section analyzes the Governor’s executive order issued in 2019 to transition Medi‑Cal’s pharmacy services benefit from managed care to entirely an FFS benefit. (Transitioning benefits from managed care to FFS is referred to as “carving out” a service.) Please see our previous report, The 2019‑20 Budget: Analysis of the Carve Out of Medi‑Cal Pharmacy Services From Managed Care, for more background on and analysis of the pharmacy services carve out. This section also analyzes the two new prescription drug affordability proposals by the Governor that primarily impact Medi‑Cal or DHCS—(1) to consider international prices in the negotiation of drug rebates and (2) to authorize DHCS to collect rebates on drugs that are not paid for through Medi‑Cal. Our forthcoming report will analyze the Governor’s two other major prescription drug affordability proposals that have a statewide implication (that is, not Medi‑Cal/DHCS‑focused)—(1) to create a California generic drug label and (2) to establish the Golden State Drug Pricing Schedule.
Background
Brand‑Name Versus Generic Drugs
A “brand‑name” drug is a drug that is sold under a trademarked name. Brand‑name drugs are often “innovator” drugs that enjoy patent protection, which prohibits nonowners of the patent from manufacturing and selling the drug without the owner’s consent. As such, brand‑name drugs are often single‑source drugs, meaning that the patent owner has no competitors offering an identical drug for sale within the drug market. A generic drug is a non‑brand‑name drug that is made with the same chemical combination as a currently or formerly available brand‑name drug that has had its patent and exclusivity period expire (usually after roughly 15 years of coming to market). Typically, generic drugs are multiple‑source drugs where multiple manufacturers compete to produce and sell drugs made of identical chemical combinations. Because brand‑name drugs often do not face any marketplace competition, they tend to be significantly more expensive than generic drugs.
Medi‑Cal Pharmacy Services
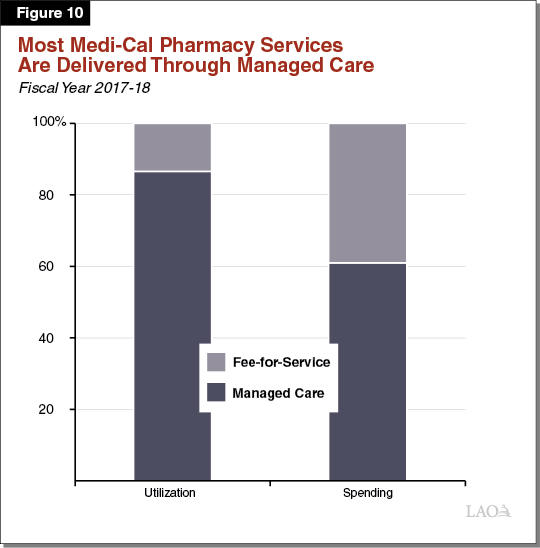
Medi‑Cal Covers Pharmacy Services, Predominantly Through Managed Care. Under its pharmacy services benefit, Medi‑Cal covers prescription drugs and other medical products obtained from pharmacies for the nearly 13 million state residents enrolled in the program. For the vast majority of Medi‑Cal recipients, Medi‑Cal pays the entire cost of covered drugs and medical products. As shown in Figure 10, most Medi‑Cal pharmacy services utilization and a majority of spending occurs through managed care. Although Medi‑Cal managed care plans currently cover and pay for most prescription drugs in Medi‑Cal, certain therapeutic classes of drugs—primarily, expensive classes of drugs, such as those for hemophilia and HIV—are carved out of managed care and instead paid for directly by the state through FFS.
DHCS Generally Only Directly Collects Supplemental Rebates in FFS. For most prescription drugs dispensed to Medi‑Cal enrollees, the state collects “federally required” rebates from drug manufacturers according to formulas prescribed under federal law. In addition, DHCS uses the Medi‑Cal program’s purchasing power to negotiate state supplemental rebates from drug manufacturers on top of the federally required rebates, but primarily only for prescription drugs paid for through FFS. Both types of rebates lower the final cost of prescription drugs. Hereafter, we refer to prescription drug costs before accounting for rebates as “gross” costs, and costs after accounting for rebates as “net” costs.
Rebates, Primarily Federally Required Rebates, Significantly Reduce Net Prescription Drug Costs in Medi‑Cal. On average, the federally required rebates lower the net cost of prescription drugs by between 30 percent and 50 percent. State supplemental rebates reduce the net cost of prescription drugs by a considerably smaller amount—around 3 percent if only counting the drugs for which the state receives supplemental rebates (those generally paid for through FFS). In addition, Medi‑Cal managed care plans also generally negotiate supplemental rebates from drug manufacturers. The savings to plans (around 4 percent) are of a similar magnitude as state supplemental rebates and are at least partially passed along to the state in the form of lower capitated payments to Medi‑Cal managed care plans.
In FFS, the State Receives Direct Savings Through the 340B Program… The federal 340B program entitles eligible health care providers (mainly hospitals and clinics that serve large numbers of low‑income patients) to discounts on outpatient prescription drugs (drugs that are not administered by a physician or within a hospital setting). These discounts result in savings that benefit participating health care providers, payers for health care such as Medi‑Cal, and other entities, such as the retail pharmacies that dispense drugs purchased through the 340B program (hereafter referred to as 340B drugs). In Medi‑Cal FFS, the state pays for 340B drugs at the purchasing hospital or clinic’s discounted cost, plus a fee to cover the cost of dispensing the drug. This means 340B discounts are passed along to the state in Medi‑Cal FFS.
…While In Managed Care, Providers Retain Earnings Through the 340B Program. In Medi‑Cal managed care, however, managed care plans pay negotiated prices for 340B drugs. This allows the health care providers participating in the 340B program to keep the difference between (1) their discounted cost and (2) the negotiated prices paid by Medi‑Cal managed care plans. Therefore, 340B savings in managed care generally accrue to hospitals, clinics, and their retail pharmacy partners rather than being passed along to the state. For more information on the interaction between the 340B program and Medi‑Cal, see our report, The 2018‑19 Budget: Analysis of the Governor’s 340B Medi‑Cal Proposal.
Governor’s January 2019 Executive Order
Carve Out Medi‑Cal Pharmacy Services From Managed Care. In early January 2019, Governor Newsom released an executive order that, among other changes, directed DHCS to carve out the Medi‑Cal pharmacy services benefit from managed care and transition it entirely to FFS. Under this carve out, DHCS would more directly pay for and manage the pharmacy services utilized by Medi‑Cal beneficiaries, in contrast to paying Medi‑Cal managed care plans to do so. The administration hopes that the carve out will enable DHCS to use the full negotiating power of the Medi‑Cal program and its nearly 13 million enrollees to negotiate deeper discounts on prescription drugs than currently achieved. At the time the executive order was released, the administration did not release an estimate of the savings that would result from the carve out.
Key 2019 Developments Related to the Carve Out. The following bullets describe the two major developments that occurred related to the Medi‑Cal pharmacy services carve out following the Governor’s executive order.
- Administration Released a Savings Estimate. In May 2019, DHCS estimated that the carve out would, on net, result in ongoing General Fund savings of $393 million on an annual basis.
- Contract Awarded to a Company to Help Administer the Carved‑Out Benefit. In November 2019, DHCS announced the awarding of a contract to an administrative services organization—Magellan Medicaid Administration, Inc.—to assist the state in administering the entire Medi‑Cal pharmacy benefit through FFS. Rather than acting as a full‑service pharmacy benefit manager, Magellan primarily will assist the state by paying pharmacy claims and performing first‑line authorizations for drugs that require administrative review before being dispensed. DHCS, rather than Magellan, will (1) set the state’s preferred drug list (the drugs that will not require administrative review, also known as prior authorization), (2) negotiate discounts with drug manufacturers, (3) make final determinations related to prior authorizations, and (4) continue to perform certain other administrative responsibilities.
Governor’s Proposal
The Governor’s budget proposes several changes to facilitate the pharmacy services carve out. In addition, the Governor proposes two novel changes to state law, more loosely related to the carve out, aimed at increasing DHCS’ power to obtain deeper discounts on prescription drugs. We describe these proposed changes in this section.
Proposals and Update Related to the Carve Out
Proposes Budget‑Related Language to Facilitate Carve Out. The Governor proposes budget‑related language aimed at improving the experience for Medi‑Cal beneficiaries under the pharmacy services carve out. This language would make two statutory changes: (1) remove the current limit in FFS of six prescriptions per Medi‑Cal beneficiary and (2) eliminate the state’s authority to collect copays for prescription drugs obtained at pharmacies.
Proposes Supplemental Payment Pool for Clinics to Mitigate Loss in 340B Earnings. As a consequence of transitioning Medi‑Cal pharmacy services from managed care to FFS, participating providers (primarily hospitals and clinics) generally will no longer be able to generate earnings through the 340B program. To mitigate the loss in earnings for clinics but not hospitals or hospital‑affiliated clinics, the Governor proposes to spend $53 million General Fund ($105 million total funds) on an ongoing basis through the creation of a new supplemental payment program. For 2020‑21, the Governor proposes half‑year funding of $26 million General Fund ($53 million total funds). The administration indicated that the supplemental payments would be made to qualifying clinics based on the prescription drug utilization of their patient populations.
Budget Assumes $43 Million in Associated Net General Fund Savings in 2020‑21, and $405 Million Ongoing. The Governor’s budget revises the administration’s previous estimate of savings under the pharmacy services carve out. On an ongoing basis, the administration now estimates $405 million in net General Fund savings under the carve out (nearly $1.2 billion total funds). The administration assumes a gradual ramp up of these savings, estimating that $43 million in net General Fund savings ($126 million total funds) will materialize in 2020‑21. Given the January 1, 2021 implementation date, the 2020‑21 savings estimate reflects a half‑year of the carve out being in effect. Figure 11 summarizes the administration’s estimate of savings under the carve out.
Figure 11
DHCS Estimate of Savings Under the
Medi‑Cal Pharmacy Services Carve Out
General Fund (In Millions)
|
2020‑21 |
Ongoing |
|
|
Direct Pharmacy Costs |
||
|
Change in gross pharmacy spending |
‑$14 |
‑$33 |
|
Additional state supplemental rebate revenue |
‑12 |
‑292 |
|
Savings on 340B drugs |
‑31 |
‑74 |
|
Subtotals |
(‑$57) |
(‑$399) |
|
Lower administrative costs |
‑$14 |
‑$58 |
|
340B clinic supplemental payment program |
26 |
53 |
|
Grand Totals |
‑$43 |
‑$405 |
|
Note: Negative numbers denote savings; positive numbers denote costs. Totals may not add due to rounding. DHCS = Department of Health Care Services. |
||
New Proposals
Authorizes Consideration of International Best Prices in Rebate Negotiations With Drug Makers. The Governor proposes budget‑related legislation to change state law so that DHCS, when negotiating state supplemental rebates from drug manufacturers, may consider the best prices manufacturers make available to international purchasers and payers. In contrast, today, state statute authorizes DHCS to consider the best prices available to domestic purchasers and payers.
Authorizes DHCS to Collect Rebates for Drugs Not Paid for by Medi‑Cal. The Governor proposes budget‑related legislation that would authorize DHCS to collect rebates for drugs that are paid for by entities other than Medi‑Cal. The intent is to utilize the purchasing power—as well as DHCS’ established infrastructure for collecting rebates—to obtain deeper discounts on prescriptions drugs. Any rebate revenues collected on behalf of non‑Medi‑Cal beneficiaries would be used to offset General Fund expenditures in Medi‑Cal, and thereby increase the amount of General Fund available to the Legislature for any other purpose by the amount of additional rebates collected. The proposed budget‑related language would give the administration the authority to determine which non‑Medi‑Cal populations would be included in the rebate program.
LAO Assessment and Recommendations
Carve Out’s Estimated Savings Are Uncertain
DHCS’ Savings Estimate Is More Comprehensive Than Last Year’s Estimate. Last year, DHCS’ estimate of savings under the carve out did not capture a major component of savings—those related to changes in how the state would reimburse 340B drugs. DHCS’ updated estimate captures at least a significant portion, but not all, of likely savings related to 340B drugs. The estimate includes likely savings on 340B drugs provided through clinics, but, due to data limitations, excludes likely savings on 340B drugs provided through hospitals.
General Fund Savings Estimate Likely Is Overstated Due to Overly Optimistic Assumptions Related to Supplemental Rebates. While DHCS’ updated savings estimate is more comprehensive than last year’s estimate, it likely significantly overstates the savings that will be generated by the carve out. Under the carve out, DHCS assumes the state will be able to more than quintuple state supplemental rebate revenues—so that they eventually reach $292 million in General Fund annually, as shown in Figure 11—without facing significantly higher gross costs for prescription drugs. DHCS believes such savings through state supplemental rebates are achievable since the state was able to collect state supplemental rebates at these levels in the mid‑2000s, before Medi‑Cal had transitioned to a program predominantly run through managed care. We believe that collection of rebates at these levels is overly optimistic absent a significant increase in gross pharmacy services costs for the following reasons:
- Significantly Higher Generic Drug Utilization. Today, around 90 percent of drugs paid for by Medi‑Cal are generic drugs. In the mid‑2000s, around 50 percent of drugs paid for by Medi‑Cal were generics. We understand that the state collects no state supplemental rebates on generic drugs. In our view, the administration’s savings estimate does not account appropriately for the significant shift away from brand‑name drugs to generic drugs that has occurred over the last 15 years or so. Accordingly, we find that the DHCS estimate likely significantly overstates savings under the carve out.
- Higher Federally Required Rebates. For many expensive prescription drugs, the ACA in 2010 amended federal law to significantly increase the minimum level of federally required rebates that drug manufacturers must pay to Medicaid programs. Given the higher level of federally required rebates, drug manufacturers are unlikely to offer state supplemental rebates as high as they did prior to the ACA’s changes to federal law.
- Medi‑Cal Managed Care Plans Achieve 4 Percent Savings. Some, though not all, Medi‑Cal managed care plans have significant prescription drug purchasing power based on their total nationwide membership. For example, Anthem has more than 40 million members nationwide while Kaiser Health Plan has around 12 million. We understand that the large Medi‑Cal plans regularly use the full negotiating power associated with their total nationwide membership to negotiate rebates from drug manufacturers. While DHCS may be able to surpass 4 percent in state supplemental rebate savings, we seriously question whether the department could do three times as well as Medi‑Cal managed care plans currently do.
- State Supplemental Rebate Estimate Is Substantially Higher Than the Percentage Amount Collected by Any Other State Medicaid Program. We understand that the most any state collects in state supplemental rebates is 7 percent of gross pharmacy services spending. DHCS’ estimate assumes the state will collect 12 percent of gross Medi‑Cal pharmacy services spending under the carve out—a rate that is 70 percent higher than what is achieved by any other state Medicaid program. While we agree that, given Medi‑Cal’s size, the state could collect state supplemental rebates at a higher rate than any other state, a rate that is 70 percent higher than any other state appears overly optimistic.
Ultimate Savings Are Highly Uncertain But Likely Lower Than Governor Estimates… Savings under the carve out are highly uncertain due to data limitations and the challenge of predicting the outcomes of future negotiations between the state, drug manufacturers, and potentially other providers. In our assessment, and as shown in Figure 12, net General Fund savings are more likely to be around $150 million annually on an ongoing basis, or between 30 percent and 40 percent of what DHCS estimates. Assuming a similar ramp‑up schedule as DHCS has assumed, we would project related savings of around $15 million in 2020‑21, as opposed to the $43 million estimated by DHCS. Our projected savings are not precise, and the fiscal impact could differ by hundreds of millions of dollars. While we view the carve out as likely to generate net General Fund savings, there is a tangible risk that the carve out could have the opposite of the intended effect and result in net General Fund costs. This risk primarily stems from two possibilities: (1) that DHCS could pursue high state supplemental rebates without necessarily achieving lower net drug costs and (2) that the costs of administering the benefit could be significantly higher than currently assumed.
Figure 12
Comparison of DHCS and LAO Estimates of Net Savings Under the Medi‑Cal Pharmacy Services Carve Out
General Fund (In Millions)
|
DHCS |
LAO |
|
|
Direct Pharmacy Costs |
||
|
Change in gross pharmacy spending |
‑$33 |
$60 |
|
Additional state supplemental rebate revenue |
‑292 |
‑160 |
|
Savings on 340B drugs |
‑74 |
‑80 |
|
Subtotals |
(‑$399) |
(‑$180) |
|
Lower administrative costs |
‑$58 |
‑$40 |
|
340B clinic supplemental payment program |
53 |
53 |
|
Other |
— |
20 |
|
Grand Totals |
‑$405 |
‑$150 |
|
Note: Negative numbers denote savings; positive numbers denote costs. Totals may not add due to rounding. DHCS = Department of Health Care Services and LAO = Legislative Analyst’s Office. |
||
…And Without New Reporting Requirements, Any Savings Will Be Difficult to Track. The actual fiscal impact of the carve out will be difficult to track through the existing fiscal reports produced by DHCS. While DHCS’ fiscal reports will provide aggregate gross and net spending totals, they will not display how pharmacy services utilization has changed—for example, if it has gone up or if utilization of brand‑name drugs has increased relative to utilization of generic drugs. Moreover, due to changes in the complex makeup of the prescription drug market, no one fiscal measure will clearly indicate whether the state has achieved savings under the carve out.
Recommend Enacting Reporting Requirements in Order to Oversee Fiscal Impact of Pharmacy Services Carve Out. Because the fiscal impact of the carve out will be difficult to assess using existing fiscal reports by DHCS, we recommend that the Legislature establish detailed reporting requirements for DHCS. Such reports are necessary to ensure that the Legislature will know the extent to which the carve out is achieving one of its primary goals—to generate savings in Medi‑Cal. Reports should compare spending on pharmacy services prior to and after the carve out, and include at least the following elements:
- Estimates of Gross and Net Pharmacy Services Spending Per Drug Prior to and After the Carve Out. Because changes in utilization could significantly impact overall Medi‑Cal spending on pharmacy services, obtaining information on spending per drug utilized will be important.
- Average Net Cost and Utilization Estimates of Top 25 Most Expensive and Top 25 Most Utilized Drugs. Because developments in the pharmaceutical market will render pharmacy services spending per drug an imperfect estimate of the fiscal impact of the carve out, a second approach to understanding changes in pharmacy services spending would be useful for understanding the fiscal impact of the carve out. As such, the Legislature could consider requiring DHCS to report net cost and utilization estimates of the top 25 most expensive and top 25 most utilized drugs in Medi‑Cal.
- Generic Versus Brand‑Name Drug Utilization and Spending. Generics are significantly less expensive than brand‑name drugs and generally equivalent in terms of efficacy. In our view, to ensure savings under the carve out, maintaining high levels of generic drug utilization in Medi‑Cal will likely be critical. Accordingly, a key measure of the carve‑out’s fiscal performance will be the degree to which generic drug utilization levels remain high. The Legislature could go further than reporting requirements and also require DHCS to release a communication each time it includes a brand‑name drug for which there is a generic equivalent on Medi‑Cal’s preferred drug list, attesting that it has performed an analysis that shows that, on net, the brand‑name drug will be less expensive than the generic competitor.
- Changes in 340B Drug Utilization. A major component of gross savings under the carve out will result from changes to 340B reimbursement. To obtain a more comprehensive picture than the administration’s estimate of what 340B savings under the carve out may be, the report should assess changes in Medi‑Cal spending on 340B drugs for all providers that utilize the 340B program.
- Estimate of Spending on Administration of the Pharmacy Services Benefit Prior to and After the Carve Out. In our view, whether proposed funding to administer the carve out will be sufficient for ongoing implementation is somewhat uncertain. In addition, existing fiscal reports produced by DHCS will not show how much funding has been removed from managed care plans’ capitated rates specifically for administering pharmacy services. Accordingly, we recommend for DHCS to annually report (1) the additional funding needed to administer the pharmacy services carve out and (2) the annualized amount of funding removed from Medi‑Cal managed care plans’ capitated rates specifically for administration.
Carve Out Implementation Time Line Is Optimistic
Many systems changes need to be completed to ensure the smooth transition of pharmacy services from managed care to FFS. Most critically, DHCS and its new administrative services contractor must be ready to receive and pay claims to almost every pharmacy in the state, as well as perform necessary prior authorizations. Delays in DHCS’ or the administrative services contractor’s readiness—without a similar delay in the effective date of the carve out—would significantly disrupt Medi‑Cal beneficiaries’ ability to obtain their prescription drugs and other medical supplies from pharmacies. However, delaying the effective date for the carve out comes with significant challenges. For one, funding for pharmacy services is scheduled to be removed from managed care plans’ capitated rates starting in January 2021. In preparation for the date of transition, managed care plans need to have plans for the winding down of their capacity to administer the pharmacy services benefit. The extent to which Medi‑Cal managed care plans will have the functional capacity to administer pharmacy services past January 2021 should the state not be ready to implement the carve out is unclear.
Recommend Requiring DHCS to Report on Progress to Date. Given the optimistic time line of implementation of the carve out, we recommend that the Legislature use the budget process to ask DHCS and stakeholders for information to assess the extent to which implementation is on track for the January 1, 2021 effective date of the carve out.
Supplemental Payments for Clinics
How Supplemental Payments for Clinics Will Be Structured Still Somewhat Uncertain. We await more information from the administration on certain specifics of how the supplemental payments will be structured. For example, at this point, how much each supplemental payment will be and how patients’ pharmacy services utilization data will flow from pharmacies to clinics and then to DHCS is unknown.
Supplemental Payments Will Significantly Reduce Net General Fund Savings Under the Carve Out. The Governor’s proposal to mitigate clinics’ financial losses under the changes related to 340B reimbursement through the creation of a supplemental payment program will partially offset a major component of savings under the carve out. According to our estimate, this proposal reduces net General Fund savings under the carve out by around 25 percent.
In the Short Run, Backfilling Lost Funding for Clinics Might Have Merit… We understand that clinics have come to rely upon 340B earnings through Medi‑Cal managed care as a major revenue source. Accordingly, eliminating these earnings, without giving clinics some time to adjust to this loss in earnings, could disrupt clinic operations and their ability to serve their patients in the short run. For this reason, temporary supplemental payments that backfill clinics’ lost earnings might have merit.
…In the Long Run, What Public Purpose the Supplemental Payments Would Serve Is Unclear. Neither federal nor state law prescribes how clinics participating in the 340B program can spend their 340B earnings. Accordingly, while clinics likely use a portion of these earnings to improve access or quality, there is no requirement that they do so. Therefore, backfilling clinics’ lost 340B earnings does not necessarily fulfill a public purpose, such as improving access or quality. Moreover, most of the clinics that would be eligible for the 340B supplemental payments receive cost‑based reimbursement from Medi‑Cal, which generally ensures that their costs are covered. Since the reimbursement methodology for clinics already covers their costs, and generally is more generous than what other Medi‑Cal providers receive, the possibility that many clinics would close—thereby significantly hurting access in Medi‑Cal—appears unlikely. Given somewhat generous reimbursement for affected clinics and the lack of an explicit link between the supplemental payments and improvements in quality or access, the value of providing these payments in the long run is unclear.
Recommend Making Supplemental Payments Temporary or, if Made Ongoing, Tie Them to Quality and/or Access Improvements. We recommend that the Legislature only approve the Governor’s proposed supplemental payments, as currently structured, on a limited‑term basis to help clinics adjust to lower revenues. Alternatively, if the Legislature wishes to provide supplemental payments to clinics on an ongoing basis, we recommend that the Legislature specifically tie the payments to improvements in either access or quality rather than on the prescription drug utilization of clinic patients.
International Best Prices
Policy Change Unlikely to Result in Any Significant Savings. In our view, DHCS currently has the authority to open negotiations with drug manufacturers by asking for any price they wish. Authorizing DHCS to consider international prices for drugs will not change this aforementioned authority. As such, we are skeptical that the policy change will result in significant new savings in Medi‑Cal.
No Major Concerns With Adopting Proposed Statutory Change. While, in our assessment, this proposed change to state law will not result in much savings for the state, there is no significant cost to making the change. Accordingly, the Legislature could consider approving the Governor’s proposed budget‑related language.
Collection of Rebates for Drugs Not Paid for Through Medi‑Cal
Policy Change Has Merit Since It Could Significantly Increase the Negotiating Power of State Drug Purchasers. We find that expanding DHCS’ authority to collect rebates on drugs not paid for through Medi‑Cal has significant merit. We believe such a change could result in state savings on prescription drugs, while also potentially streamlining state negotiations on drug prices.
Outstanding Questions. At this time, on which populations’ behalf DHCS would negotiate non‑Medi‑Cal prescription drug rebates is unclear. However, we expect that these non‑Medi‑Cal populations could include, for example, incarcerated individuals, Department of Developmental Services consumers, and students in the California State University system. In addition, the proposed legislation does not require the administration to notify the Legislature of decisions on which populations will be included in the rebate program. Finally, there is uncertainty as to how adding populations might affect which drugs are made available to the various participating populations.
Recommend Approving in Concept. Given the potential of this proposal to generate savings and streamline negotiations on drug prices, we recommend approval of the Governor’s proposal to authorize DHCS to collect rebates on drugs not paid for through Medi‑Cal—contingent upon the administration answering certain outstanding questions during the budget process. We recommend that the Legislature ask the administration how it intends to decide on the appropriateness of adding populations to the rebate program and how the Legislature will ultimately be informed of such decisions.
Full‑Scope Expansion for Seniors Regardless of Immigration Status
Background
Prior to 2015, Undocumented Immigrants Were Eligible Only for “Restricted‑Scope” Medi‑Cal Coverage. Medi‑Cal eligibility depends on a number of individual and household characteristics, including, for example, income, age, and immigration status. Historically, income‑eligible citizens and immigrants with documented status have qualified for comprehensive, or “full‑scope,” Medi‑Cal coverage, while otherwise income‑eligible undocumented immigrants generally have not qualified for full‑scope Medi‑Cal coverage. Rather, those who would be eligible for Medi‑Cal but for their immigration status were historically eligible only for restricted‑scope Medi‑Cal coverage, which covers emergency‑ and pregnancy‑related health care services. The federal government pays for a portion of undocumented immigrants’ restricted‑scope Medi‑Cal services according to standard FMAP rules.
Today, Otherwise Eligible Young Undocumented Immigrants Are Eligible for Full‑Scope Medi‑Cal Coverage. In 2016, the state expanded full‑scope Medi‑Cal coverage to otherwise eligible undocumented children from birth through age 18. Then, in the 2019‑20 budget, the state expanded full‑scope Medi‑Cal coverage to otherwise eligible undocumented young adults ages 19 through 25. Today, undocumented immigrants ages zero through 25 are eligible for full‑scope Medi‑Cal coverage. Undocumented adults ages 26 and over currently are only eligible for restricted‑scope Medi‑Cal coverage.
Undocumented Immigrants Continue to Represent a Significant Portion of the State’s Remaining Uninsured Population. Undocumented immigrants above age 25 do not qualify for public financial assistance to obtain comprehensive health care coverage, either through Medi‑Cal or through the state’s Health Benefit Exchange known as Covered California. As a result, they represent a significant portion of the state’s remaining uninsured. Recent estimates indicate that there are likely more than 1.5 million uninsured undocumented immigrants in the state, which represents as much as 50 percent of the state’s remaining uninsured. Figure 13 provides a brief overview of where the state stands today in terms of Medi‑Cal coverage of undocumented immigrants, including an estimate of the General Fund cost to expand full‑scope Medi‑Cal coverage to otherwise eligible populations not currently covered or proposed to be covered by the Governor.
Figure 13
Ongoing Caseload and Cost of Expanding Full‑Scope Medi‑Cal Coverage to Otherwise Eligible Undocumented Immigrants
|
Coverage and Age Groups |
Caseload |
General Fund Cost (In Millions)a |
|
Populations That Currently Have Full‑Scope Coverage |
||
|
Otherwise eligible children ages 0‑18 |
130,000 |
$150 |
|
Otherwise eligible adults ages 19‑25 |
105,000 |
260 |
|
Population Proposed to Gain Full‑Scope Coverage in 2020‑21 |
||
|
Otherwise eligible seniors ages 65+ |
27,000 |
250 |
|
Remaining Population Only Eligible for Restricted‑Scope Coverage |
||
|
Otherwise eligible adults ages 26‑64b |
890,000 |
2,350 |
|
All |
1,150,000 |
$3,000 |
|
aCost estimates include those in both Medi‑Cal and the In‑Home Supportive Services programs. bShould the Legislature approve the Governor’s proposed expansion for undocumented seniors ages 65 and older, the 26‑64 year old age‑group reflects the caseload and cost of expanding to the remaining uninsured, otherwise eligible undocumented immigrants. |
||
Governor’s Proposal
Expand Full‑Scope Medi‑Cal Coverage to Otherwise Eligible Undocumented Seniors Ages 65 and Older. The Governor’s budget proposes to expand full‑scope Medi‑Cal coverage to otherwise income‑eligible undocumented seniors 65 and older. Nearly 27,000 seniors are expected to gain full‑scope coverage under the expansion. The Governor’s budget projects that around $64 million General Fund ($80 million total funds) will be needed to fund the expansion in 2020‑21, which is proposed to begin halfway through the fiscal year in January 2021. Of this General Fund amount, $58 million reflects funding in Medi‑Cal through DHCS and $6 million reflects funding in the In‑Home Supportive Services (IHSS) program through the Department of Social Services. On an ongoing annual basis, the Governor projects this expansion will cost around $320 million General Fund, split close to evenly between Medi‑Cal and IHSS. Whereas the administration expects the full Medi‑Cal costs to materialize within a year of implementation, it expects IHSS costs to gradually grow over several years until reaching around $150 million General Fund in 2022‑23.
Assessment
Governor’s Fiscal Estimate Appears Reasonable. Overall, the Governor’s caseload and cost estimates for the undocumented seniors expansion generally appear reasonable in 2020‑21. However, the multiyear caseload and cost impact—in IHSS in particular—might turn out to be lower than what is assumed by the administration, particularly given the speed by which the administration assumes them to grow over time. That said, we do not recommend any changes to the Governor’s budget assumptions at this time. Figure 13 summarizes the Governor’s projected ongoing General expenditures for the proposed undocumented seniors expansion, and compares this year’s proposal to (1) previous expansions for the undocumented population and (2) the caseload cost of expansion to the remaining undocumented population that could be eligible for full‑scope Medi‑Cal coverage.
SNF Rate Reform
Background
SNF Spending Makes Up Significant Share of Medi‑Cal Budget. SNFs provide medical, rehabilitative, and skilled nursing care for those who cannot receive such care in a home setting. SNF care is a covered benefit in Medi‑Cal and makes up a large amount—we estimate roughly $5 billion (total funds)—of Medi‑Cal expenditures. Currently, there are over 1,000 licensed SNFs in the state. Medi‑Cal payments are a significant revenue source for SNFs. Statewide, the majority of SNF residents are covered by Medi‑Cal.
Medi‑Cal Rates for SNFs Set Under Cost‑Based Framework. The state’s current framework for setting SNF reimbursement rates initially was put in place through Chapter 875 of 2004 (AB 1629, Frommer). The framework established by Chapter 875 assigns each SNF an individual rate each year based on its reported costs from two years prior, with some adjustments. First, DHCS adjusts downward reported costs if they exceed statutorily defined ceiling amounts. As shown in Figure 14, these ceilings are determined relative to reported costs of other SNFs in a “peer group” that the state established to group similarly situated SNFs. The cost ceilings are intended to provide an incentive for SNFs to control the growth of their costs relative to other SNFs in the peer group. Next, DHCS caps the growth in the cost‑based rates so that overall SNF rates do not increase by more than 3.62 percent on average. Without this cap, SNF rates typically would grow by more than 3.62 percent, so, in practice, SNFs have received an average annual increase of 3.62 percent in recent years.
Figure 14
Cost Ceilings for SNF Rates
|
SNF Costs for These Items... |
Are Limited to... |
|
Direct care labor |
90th percentile of peer group costs |
|
Indirect care labor |
90th percentile of peer group costs |
|
Direct and indirect nonlabor |
75th percentile of peer group costs |
|
Administration |
50th percentile of peer group costs |
|
Professional liability insurance |
75th percentile of peer group costs |
|
Property taxes |
No limit |
|
Licensing fees |
No limit |
|
Caregiver training |
No limit |
|
QAF |
No limit |
|
Fair rental valuea |
No limit |
|
aThe state has a separate process for determining fair rental value for SNFs. SNF = skilled nursing facility and QAF = quality assurance fee. |
|
General Fund Costs for SNF Care Partially Offset by QAF. Chapter 875 also established a QAF that SNFs pay to the state to offset the General Fund costs of the rates paid under the cost‑based framework described above.
SNFs Also Receive Quality Incentive Payments. In 2010, the Legislature adopted the Quality and Accountability Supplemental Payment (QASP) program, which provides incentive payments to SNFs based on their performance on specified performance measures. For 2019‑20, the total amount of incentive payments is limited to $88 million. The cost for the supplemental payments is shared roughly equally by the federal government and state funds, with state funds coming almost entirely from the General Fund.
State Authorization for Rate Framework, QAF, and QASP Expires in August 2020. When Chapter 875 was enacted, it included a statutory “sunset” date after which the cost‑based reimbursement methodology and QAF would be repealed. The Legislature has since extended the sunset date multiple times, while making some changes in the structure of the rate‑setting methodology and the QAF. Under the most recent extension, the rate framework and the QAF will sunset in August 2020. The QASP also sunsets in August 2020.
2018 State Audit Raised Concerns About SNF Quality and QASP’s Effectiveness. In 2018, the California State Auditor released a report on quality of care, financial practices, and statewide oversight of SNFs. Among other things, the report identified a growing number of findings of quality deficiencies at SNFs from 2006 through 2015 and concluded that the QASP program was not as effective as it could be due to its relatively limited size and the number of facilities that could receive an award.
SNF Care Currently Is Covered Under Managed Care in Certain Counties. Prior to 2013, the Medi‑Cal SNF benefit was provided as a Medi‑Cal FFS benefit in most counties, meaning the state paid SNFs directly based on the rates determined under the rate‑setting framework described above. Beginning in 2013, the Medi‑Cal managed care plans began paying for the SNF benefit in seven of the state’s most populous counties—Los Angeles, Orange, Riverside, San Bernardino, San Diego, San Mateo, and Santa Clara. (These counties are home to more than 50 percent of Medi‑Cal beneficiaries.) This shift was done as part of the Coordinated Care Initiative, a demonstration project aimed at increasing the integration of care for seniors and persons with disabilities, particularly those dually eligible for Medi‑Cal and Medicare. In counties where SNF care is provided through managed care, managed care plans have the ability to pay a rate other than the state FFS rate, but plans generally have paid SNFs the FFS rate determined through the rate‑setting methodology described above. However, in some limited cases, plans have agreed with SNFs to pay a higher rate.
Governor Proposes Fully Moving SNF Benefit Into Managed Care. As part of MHCA, the Governor has proposed to move SNF care from FFS to managed care statewide. Under the Governor’s proposal, this transition would be effective beginning January 2021. We assess this proposal in a forthcoming report analyzing the administration’s MHCA proposal.
Overview of the Governor’s Proposal
Governor Proposes Reauthorizing Rate‑Setting Framework and QAF, With Several Changes. The Governor proposes to extend the sunset date for the SNF reimbursement methodology and QAF to the end of December 2024, with several changes that are described below.
Increases Overall Cap on Annual Rate Growth. In budget documents released January 10, 2020, the Governor proposed to provide an aggregate rate increase consistent with the current 3.62 percent cap in August 2020, with an additional midyear increase of 1.5 percent effective January 2021. The administration estimated this midyear rate increase would result in General Fund costs of around $50 million (General Fund). After the release of the budget, the administration indicated it has revised its proposal to instead provide a midyear increase of 3.5 percent, but has not provided an updated cost estimate. The Governor further proposes to provide 4 percent increases in 2022, 2023, and 2024 (after which the revised rate framework would sunset, unless reauthorized).
Extends QASP One Year, Then Eliminates QASP and Conditions Portion of Rate Increases on Quality. The Governor proposes to make QASP payments for one additional year in 2021 based at the same level of total funding ($88 million). After 2021, the QASP would be eliminated. Instead, beginning in 2022, a portion of each SNF’s calculated rate increase under the 4 percent cap would be placed in a “quality pool,” from which SNFs could only earn their full rate increase contingent on meeting quality expectations. The portion of rate increases that would be placed in the quality pool and the allocation of quality pool funds are described in Figure 15.
Figure 15
New SNF Quality Framework Under Governor’s Proposal
|
Portion of Aggregate Rate Increase Allocated to Quality Pool |
|
|
2022 |
40% |
|
2023 |
45 |
|
2024 |
45 |
|
Distribution of Quality Pool |
|
|
|
|
|
|
|
|
SNF = skilled nursing facility. |
|
Increases Emphasis on Direct Labor Costs in Rates. The proposal would allow for higher direct labor costs in the cost‑based portion of the rate‑setting methodology by increasing the cost ceiling from the 90th percentile to the 95th percentile.
Increases the Number of Peer Groups for Determining Cost Ceilings. The Governor proposes to increase the number of peer groups to determine cost ceilings from the current number of 7 to 12. The administration indicates this change is proposed to take into account changes in the distribution and operations of SNFs since the peer groups were initially established, to increase the degree to which SNFs within a peer group are similarly situated.
Would Set State‑Determined Rates as Floor for Managed Care Payments. The Governor proposes to specifically require Medi‑Cal managed care plays to pay SNFs the rate determined under the proposed revised rate‑setting framework, unless the managed care plan and the SNF mutually agree to a different, higher rate.
Increases Authority to Collect Delinquent QAF. Finally, the Governor proposes changes to increase QAF collections from providers that have not remitted the payment as required. Specifically, the Governor proposes to:
- Allow DHCS to assess penalties and interest for QAF payments that are past due.
- Allow DHCS to require SNFs to provide information about other entities or facilities that have certain financial relationships (such as being owned or operated by the same parent organization) in order for DHCS to offset Medi‑Cal payments to those entities to recover past due QAF payments. (The department already withholds Medi‑Cal payments to SNFs that are past due on QAF obligations.)
- Prohibit organizations that operate SNFs from purchasing additional facilities until they have paid any past due QAF amounts or set up a plan with DHCS to repay past due QAF.
Excludes Freestanding Pediatric Subacute Facilities (FS‑PSAs) From QAF Requirement. FS‑PSAs provide specialized care for children who are dependent on medical technology (typically ventilators) for survival. There currently are only four FS‑PSAs in the state. FS‑PSAs are currently subject to the same QAF as SNFs, but do not receive rates under the cost‑based rate methodology used for SNFs. The estimated QAF revenue from these facilities is just over $1 million. The Governor proposes to no longer assess the QAF on FS‑PSAs.
LAO Assessment
In Concept, Integrating Quality Incentives in Rates Could Strengthen Positive Incentives… We estimate that the value of the quality pool (the portion of rate increases that would be conditional on quality) will not be significantly larger than the funding currently available for QASP. However, the implications of meeting or not meeting quality expectations under the Governor’s proposal could be more enduring than under the QASP. Under the QASP, SNFs receive one‑time incentive payments based on their performance, but these payments have no impact on future rates. In contrast, under the Governor’s proposal, increased payments based on meeting quality expectations would be built into the rate and form the basis on which future rate increases would be applied. In the same way, SNFs that do not meet quality expectations would have a lower rate on which future rate increases would build, perpetuating the impact of not meeting quality expectations into the future. This feature of the Governor’s proposal increases the incentive for SNFs to meet quality expectations relative to the QASP.
…But Might Also Perpetuate Low Quality by Permanently Reducing Rates. However, at the same time, SNFs that experience lower rate increases than expected after not meeting quality expectations might struggle to improve in light of the lower funding they receive. Building the loss of quality‑based payments into the rate could make it more difficult for lower‑quality facilities to improve over time.
Proposal to Use FFS Rates to Incentivize Quality Improvements Is Somewhat Unconventional. In general, the state delegates to managed care plans the responsibility of determining provider rates and overseeing the quality of providers and determining reimbursement rates. In some cases, managed care plans pay providers based on the rate the provider would receive in the FFS delivery system, but in other cases managed care plans pay higher rates in order to guarantee access to services or to provide quality incentives. This leads to providers receiving different reimbursements in different parts of the state, based on local circumstances. The Governor’s proposal to establish a complex new FFS rate‑setting structure for a benefit that is proposed to be moved fully into managed care diverges from this conceptual framework.
Transition to Managed Care Could Blunt Policy’s Impact… The potential effects of the Governor’s proposed changes described earlier depend on SNFs being paid the FFS rate that the new framework would determine for each facility. Over time, managed care plans may make arrangements with SNFs to pay different, higher rates than would be paid under FFS. To the extent that managed care plans pay higher rates than are determined through the Governor’s proposed rate framework, the impact of the Governor’s proposed changes could be lessened. For example, if a plan agrees to pay a rate to an SNF that is above the SNF’s FFS rate, then the rate paid by the managed care plan might not necessarily change in response to changes in the facility’s floor FFS rate due to that facility meeting or not meeting quality expectations. This would break the link between an SNF’s performance on quality measures and the rate that it receives, eliminating much or all of the rate structure’s incentive effect.
…But Could Give State Greater Control Over Quality Incentives, Provided Most Managed Care Plans Pay FFS Rates. Although the Governor’s proposal would allow managed care plans to pay above the FFS rate, in many cases they likely would not do so, at least initially. If managed care plans continue to mostly pay the FFS rate, the new system would retain its incentive effects. This would give the state greater control over quality incentives than it typically would have for a managed care benefit. For other types of services in managed care, the state’s conceptual approach to promoting quality is to measure the performance of managed care plans and hold plans accountable for their performance. However, in recent years, concerns have been raised about the effectiveness of the state’s oversight of managed care plans performance. The Governor’s proposal could provide a more direct way for the state to put in place quality incentives for SNF care, provided that most managed care plans pay FFS rates to SNFs.
Rationale for Some Features of Governor’s Proposal Is Unclear. The Governor’s proposal reflects several choices on the part of the administration that affect how much the reformed rate‑setting system would cost the state and what incentives the new system would create for SNFs. The rationale for some of these choices is not clear and more information is needed for legislative consideration. We identify three key areas where the rationale for a key policy choice is unclear:
- First, the administration has not clearly laid out how the amount of the midyear rate increase in 2020‑21 and the annual increases thereafter were chosen or provided a clear justification for why this level of increase should be provided, such as a need to increase rates to improve access to SNF services.
- Second, the administration has not clearly laid out why it is proposing to increase the ceiling on SNFs’ reported costs on direct labor from the 90th percentile to the 95th percentile.
- Finally, the administration has not clearly laid out how it determined amounts related to the new quality pool. This includes how the portion of the aggregate rate increase that would be allocated to the quality pool was determined. It also includes how the percentage allocations within the quality pool—between additional increases to SNFs based on their individual performance, increases to SNFs with the most improvement in their performance, and increases to SNFs with the highest performance—were determined.
Obtaining additional information on the rationale for these policy choices will be important as the Legislature considers the effects that the proposed revised rate‑setting system will have on SNFs and on the state budget.
Increased Enforcement of QAF Collections Could Offset General Fund Costs, but Impact Uncertain. As described previously, QAF revenues serve to offset the General Fund costs of SNF payments. Increasing the collection of delinquent QAF payments that otherwise would not be collected would result in General Fund savings, provided the cost of increased enforcement actions would be less than the increased QAF collected. However, little information on QAF collections is publicly available, so we are unable to estimate the possible budgetary impact of changes to increase QAF collections.
Recommendations
Withhold Action on Proposal Until More Details Are Provided. As of the writing of this analysis, many details on the Governor’s proposal were yet to be determined, such as which quality measures would be used and the specific ways SNF performance relative to these measures would inform quality‑based increases in their rates. These details could significantly affect the incentives created for SNFs that are paid the FFS rate. Additionally, the rationale for some policy choices the administration made in crafting its proposal are not clear. We recommend that the Legislature withhold action on this proposal until more details on how the proposal would be structured and why the administration made the policy choices it did in structuring its proposal. Some key questions for legislative consideration include:
- How were the amounts for the proposed midyear rate increase in 2020‑21 and later annual rate increases determined? Were these amounts chosen in response to an evaluation of levels of access or quality at SNFs for Medi‑Cal beneficiaries?
- Why is the administration proposing to increase the cost ceiling for direct care labor from the 90th percentile to the 95th percentile? What problem is this change intended to address?
- On what basis did the administration choose the amounts of the annual rate increases that would be allocated to the quality pool and how the amounts in the quality pool would be allocated to SNFs?
Ask Administration to Justify the Use of FFS Rate‑Setting Structure to Implement Quality Incentives for a Managed Care Benefit. Given the potential for the transition to managed care to blunt the quality incentive impacts of the proposed methodology, we recommend that the Legislature ask the administration to justify further at budget hearings the use of FFS rates as a tool to promote quality for a managed care benefit. Some key questions for the Legislature’s consideration include:
- Under what conditions would managed care plans be expected or allowed to pay rates above the state FFS rate determined under the proposed new rate‑setting system?
- How often would managed care plans be expected to pay higher rates?
- Are there alternative structures for providing incentives through managed care that would guarantee that SNF compensation would change based on performance relative to quality measures?
If Adopted, Require Evaluation of New Rate Structure’s Impact on Quality. If the Governor’s proposal is adopted, we recommend that the Legislature require DHCS to evaluate how the new structure affects SNF quality and report back to the Legislature. Such an evaluation could examine such questions as:
- How often and in what circumstances do managed care plans pay rates above the state FFS rate?
- To what extent did changes in SNF performance on quality measures actually translate into the rates that SNFs received from managed care plans?
- Following implementation, what evidence exists on the impact of the new rate‑setting framework on SNF quality?
Ask Administration to Comment on Current Status of QAF Collections and Potential Budgetary Impact of Enhanced Collection Tools. We recommend that the Legislature ask DHCS to provide additional information at budget hearings on (1) the current extent of delinquent SNF payments, (2) the department’s current approach to collecting delinquent QAF revenues and the effectiveness of this approach, and (3) the potential budgetary impact of the proposed new collection tools.
County Administration
Background
Counties Administer Medi‑Cal Eligibility and Enrollment Functions. Counties are responsible for eligibility and enrollment functions in Medi‑Cal. This includes things like determining individuals’ initial eligibility to enroll in the program, maintaining accurate records on individuals’ ongoing eligibility, and administering regular eligibility redeterminations. Counties also are responsible for similar functions in major human services programs, including California Work Opportunity and Responsibility to Kids (CalWORKs), CalFresh, and IHSS. Counties primarily rely on a set of information technology (IT) systems collectively referred to as the county Statewide Automated Welfare System (SAWS) to determine eligibility and maintain enrollee records. However, eligibility and enrollment processes also require counties to interact with state‑operated IT systems including the Medi‑Cal Eligibility Data System (MEDS), which is a statewide database that stores information on individuals receiving public benefits, and the California Healthcare Eligibility, Enrollment, and Retention System (CalHEERS), which supports eligibility and enrollment for health benefits through Covered California and Medi‑Cal.
Historically, County Administration Funding Determined Through Cost‑ and Caseload‑Driven Methodology…State law requires DHCS to maintain a methodology for budgeting for county Medi‑Cal administrative costs. Historically, DHCS has budgeted for county administrative expenses by determining a base amount of funding by reviewing county costs in three main areas: (1) staff costs, (2) support costs, and (3) staff development costs. The historical DHCS methodology also made adjustments for caseload, an annual cost‑of‑living adjustment (COLA), and program changes. However, the state has deviated from this practice in many instances. For example, the annual COLA for the county administration budget was suspended most years from 2008‑09 through 2017‑18 due in part to state General Fund budget shortfalls.
…And County Performance Overseen Through “County Performance Standards.” State and federal law require DHCS to oversee the counties’ eligibility and enrollment performance and state law lays out certain performance standards. These standards are listed in Figure 16. Historically, DHCS monitored the performance of the 25 counties with the largest Medi‑Cal enrollment through a process known as County Performance Standards. Under this process, counties were required to submit an annual report to DHCS on their performance relative to the standards. DHCS also has conducted periodic oversight visits as part of County Performance Standards.
Implementation of ACA Significantly Impacted County Workload. Beginning in January 2014, the state expanded eligibility for Medi‑Cal to include childless adults that previously had not been eligible to enroll. The state also began implementing new rules for determining Medi‑Cal eligibility for most enrollees known as “modified adjusted gross income,” or MAGI. These MAGI rules are simpler and more streamlined compared to preexisting eligibility rules.
Figure 16
County Administration Performance Standards
|
|
|
|
|
|
|
|
MEDS = Medi‑Cal Eligibility Data System. |
As noted earlier in this report, the ACA expansion led to a dramatic surge in enrollment in Medi‑Cal. At the same time, counties experienced significant IT‑related challenges, particularly with the interface between SAWS and the newly developed CalHEERS. These combined factors resulted in significantly increased county workload. In light of the increased workload, the state (1) suspended the County Performance Standards oversight process, (2) directed counties to prioritize enrollment of newly eligible enrollees over other functions such as redetermination and processing discrepancies between MEDS and SAWS, and (3) provided increased funding for county administration. From 2012‑13 to 2017‑18, total funding for county administration in Medi‑Cal grew from $1.4 billion ($639 million General Fund) to $2.2 billion ($778 million General Fund). These augmentations largely were determined through budget negotiations between the state and counties on a year‑by‑year basis rather than through a clearly defined methodology looking at factors such as caseload or cost per case for administration.
2018 Audit Findings Highlight Administrative Challenges. In 2018, both the California State Auditor and the Office of the Inspector General of the federal Health and Human Services Agency released audit reports that identified problems with county eligibility determinations and other administrative processes. In particular, the California State Auditor found that unresolved discrepancies between SAWS and MEDS after the ACA expansion led to significant payments being made for individuals who were potentially not eligible for Medi‑Cal, including some instances of payments made to Medi‑Cal managed care plans for Medi‑Cal beneficiaries who were deceased. DHCS is required to take actions to address the identified deficiencies as a result of these audits. As part of these efforts, the department has engaged in “fiscal performance reviews” with counties to address high‑priority deficiencies, such as those related to SAWS and MEDS discrepancies.
Current Law Directs DHCS to Develop and Implement New Budgeting Methodology for County Administration No Sooner than 2015‑16. Current law requires DHCS to develop a new methodology for budgeting county Medi‑Cal administration that would reflect the impact of changes under the ACA. This requirement initially called for the new methodology to be developed by 2012, but was delayed to accommodate other priorities during the ACA implementation period. Currently, the law does not place a deadline on DHCS to develop the new methodology, but rather specifies that the new methodology be developed no sooner than 2015‑16.
New Budgeting Methodology Has Not Been Developed. As part of the 2014‑15 budget package, DHCS received two limited‑term positions and contract funding to prepare for developing a new budgeting methodology. These resources were used to begin the process of developing a new methodology, but these plans were put on hold after the state and the counties determined that there were too many changes being made to county eligibility and enrollment processes to effectively develop a new methodology at that time. As part of the 2017‑18 budget package, these resources were extended through June 2020. After this most recent extension, the department prepared a request for proposal to bring on a contractor to assist with gathering information to develop a revised methodology for Medi‑Cal administration, but a suitable contractor was not identified and plans to revise the budgeting methodology were again put on hold. To date, DHCS has not developed a new budgeting methodology.
In the meantime, the 2018‑19 budget reset counties’ administrative base funding to be roughly equivalent to the total amounts provided during the ACA expansion. The 2018‑19 budget also returned to the practice of providing an annual COLA. This practice was continued in the 2019‑20 budget. These actions, while not establishing a new methodology per se, did increase counties’ base funding amount.
Methodologies to Budget Administrative Costs for Other Major Health and Human Services Programs Recently Revised or Soon to Be Revised. The 2018‑19 budget package included the adoption of revised budgeting methodology for county administrative costs in CalWORKs and IHSS. As part of his 2020‑21 budget proposal, the Governor stated his intent to put forward a revised budgeting methodology for CalFresh administration as part of the May Revision. The details of these revisions have varied by program, but each program’s budgeting methodology relies at least to some degree on projections or assumptions about the cost of performing administrative activities and the volume of activities to be performed.
Overview of the Governor’s Proposal
Similar to Recent Years, Provides COLA for County Administration Funding. The Governor’s budget proposes $2.4 billion in total funds ($640 million General Fund) for county administration of Medi‑Cal in 2020‑21. This includes a 3.25 percent COLA, at a cost of $68 million totals funds ($34 million General Fund).
Proposes Repurposing Temporary Positions Provided to Develop New Budgeting Methodology for Ongoing County Oversight Workload. As described earlier, DHCS received temporary positions and funding to develop a new budgeting methodology for county Medi‑Cal administration as required by law. As plans to develop this new methodology have been put on hold, these resources have been repurposed to perform county performance oversight in connection with addressing recent audit findings. The Governor proposes to make these resources—$279,000 total funds ($139,000 General Fund) for two positions—permanent in order to continue this county oversight work and to support the additional steps described below. The Governor’s proposal outlines no new plans for revising the Medi‑Cal county administration budgeting methodology.
Plans to Reinstate County Performance Standards… As part of the MHCA proposal, DHCS announced its intention to reinstate County Performance Standards. Under DHCS’ proposed time line, the department will outline an updated process for monitoring County Performance Standards during 2020 and would begin evaluating county performance relative to the standards beginning in January 2021.
…And Implement Additional Accountability Tools. DHCS further proposes to implement a county performance monitoring dashboard that makes information on county performance relative to County Performance Standards and other potential measures yet to be identified public. DHCS also proposes to begin using a tiered corrective action approach with counties that do not meet performance expectations, including corrective action plans, providing technical assistance, and assessing fiscal penalties on counties that are not responsive to requirements for improved performance. (DHCS already has the ability to require counties to enter into corrective action plans and assess fiscal penalties.)
LAO Assessment
Counties Continue to Struggle With Performance Goals. While efforts have been made to address audit findings, counties continue to fail to meet some performance standards identified in state law. For example, in April 2019, only three counties completed more than 90 percent of annual redeterminations by the month they were due (the state requirement) and 11 counties completed less than 70 percent by the due month.
Increased Oversight and Transparency of County Performance Is Warranted. Factors largely beyond the state’s and counties’ control during the period of implementing the ACA made meeting state performance standards very challenging. However, the Medi‑Cal caseload has since stabilized and many IT challenges that increased county workload have been addressed. In light of recent audit findings, now is an appropriate time to increase focus on county performance. Currently, public information on county performance, particularly on some standards such as resolving discrepancies between SAWS and MEDS, is limited. Increasing the transparency of county performance information would help the Legislature in its oversight of Medi‑Cal operations and could provide additional encouragement to low‑performing counties to improve.
Questions Remain About Administration’s Proposed Next Steps. While increased focus on oversight of county Medi‑Cal administration is laudable, many questions remain about the administration’s proposed approach.
- Which Are the Right Performance Measures? The current County Performance Standards were developed prior to implementation of the ACA. The Legislature could consider whether these measures continue to be the most appropriate measures, or whether other measures would be more appropriate in addition to or in place of current measures.
- What Are the State’s Priorities for Improving County Performance? Given the complexity of Medi‑Cal administration and the number of issues identified in state audits, counties might not be able to improve their performance on the full array of state standards all at once. The Legislature could consider establishing priorities for which areas of performance to focus on first.
- Do Counties Have an Appropriate Level of Resources Relative to the State’s Expectations? As described below, in light of changes brought about by the ACA—both those that increased workload and those that streamlined processes—whether the amount of funding provided to counties is at an appropriate level to allow counties to meet the state’s performance expectations is unclear.
- Does DHCS Have an Appropriate Level of Resources to Perform Effective County Oversight? The Governor’s proposal requests the extension of limited‑term funding for two positions to help support state oversight of county performance. However, given the breadth of the administration’s proposal related to county oversight, the Legislature may wish to comprehensively review what resources DHCS dedicates to these functions and assess whether overall funding and staffing for county oversight is at an appropriate level.
Current County Administration Budgeting Practice Lacks Strong Analytical Basis. Historically, Medi‑Cal county administration budgeting was based on a variety of objective factors, including base county staff costs, support costs, and staff development costs, with adjustments for changes in program caseload, inflation, and program changes. But over time, the role of these objective factors has diminished. Today’s base amount of funding reflects a patchwork of historical amounts and one‑time augmentations to accommodate the ACA expansion. As a result, whether the amount of funding that counties currently receive is appropriate to cover the costs of performing their responsibilities is unclear. Further, changes in county eligibility processes brought about through the ACA such as the introduction of MAGI rules—many of which streamlined eligibility requirements—mean that previous methods and assumptions used to budget county administrative funding likely are no longer adequate.
Recommendations
Withhold Action on Making Temporary Resources Permanent. We recommend that the Legislature withhold action on the administration’s request to make temporary resources permanent, pending additional information from the administration described below.
Require DHCS and Counties to Update Legislature at Budget Hearings on Current Performance and Plans for Future Changes. We recommend that the Legislature direct DHCS and counties to update the Legislature at budget hearings on current county performance and plans for changes to state oversight in the coming months. Specifically, we suggest that DHCS and counties be asked to comment on:
- The status of state and county efforts to address recent audit findings.
- The administration’s thinking in regards to timing of required revisions to the county Medi‑Cal administration budgeting methodology.
- How county spending patterns have changed in recent years as the caseload has stabilized and some IT‑related challenges have been resolved.
- Which additional performance measures should be considered.
- How planned and in‑process changes to major IT systems used in eligibility and enrollment functions affect plans for increased county oversight and potential future changes to the budgeting methodology for county Medi‑Cal administration.
Adopt a Plan for Revising Medi‑Cal County Administration Budgeting Methodology. Given the lack of a strong analytical basis for the state’s current practices for budgeting county administrative funding, we recommend the Legislature take steps to move toward a more objective budgeting approach. In our view, the current statutory requirement that DHCS develop a new budgeting methodology no sooner than in 2015‑16 provides too much discretion to the administration and limits legislative oversight of this process. We recommend that the Legislature adopt language to establish, in consultation with DHCS and counties, a specific time frame for developing a new budgetary methodology in the coming years.
Proposal to End Dental Managed Care in the Two Pilot Counties
Background
Medi‑Cal Covers Dental Services, Predominantly on an FFS Basis. Dental services are a covered benefit under Medi‑Cal. The vast majority of Medi‑Cal dental services are paid for on an FFS basis. As a predominantly FFS benefit, DHCS, with the help of an administrative services organization, arranges and directly pays for the dental services utilized by Medi‑Cal members. Accordingly, DHCS sets Medi‑Cal dental services reimbursement rates and maintains a “network” of enrolled providers.
Dental Managed Care Currently Operates in Only Los Angeles and Sacramento Counties. In 1992, the Legislature authorized the creation of a pilot program in two counties—Los Angeles and Sacramento—implementing dental managed care. Under dental managed care, private specialty managed care plans arrange and pay for dental services in place of DHCS. As specialty plans, dental managed care plans are separate from the Medi‑Cal managed care plans through which physical health care coverage is predominantly provided in Medi‑Cal. Similar to Medi‑Cal managed care plans more broadly, the state makes per member per month payments to dental managed care plans that are intended to cover the average cost of plan members’ dental services utilization. Such payments—also known as capitated payments—also are intended to cover dental managed care plans’ costs of administering the benefit. Currently, six dental managed care plans are in operation across Los Angeles and Sacramento Counties, collectively covering about 800,000 Medi‑Cal beneficiaries. In Sacramento County, enrollment in a dental managed care plan is mandatory for Medi‑Cal beneficiaries, while in Los Angeles County, Medi‑Cal beneficiaries have the option of obtaining their Medi‑Cal benefits either through dental managed care or FFS. In Los Angeles County, about 10 percent of Medi‑Cal enrollees have opted to obtain their dental benefits through dental managed care.
Governor’s Proposal
End Dental Managed Care and Return to FFS in Pilot Counties. The Governor has proposed budget‑related legislation that would end dental managed care in the pilot counties, and, instead, have all Medi‑Cal beneficiaries statewide access dental services exclusively through FFS. The administration cites ongoing performance challenges among dental managed care plans as the rationale for the proposal. In addition, the proposal is consistent with the broader MHCA reforms insofar as it standardizes service delivery on a statewide basis.
Transition From Dental Managed Care to FFS Is Intended to Be Cost Neutral. While the budget assumes nearly $9 million in General Fund savings associated with the transition from dental managed care to FFS in 2020‑21, these savings arise from the timing of payments rather than a projection of ongoing savings under statewide dental FFS. On an ongoing basis, the administration assumes that the transition to FFS will be cost neutral due to expected higher utilization of dental services following the transition offsetting higher administrative costs under dental managed care.
Proposal Does Not Affect San Mateo Health Plan Dental Integration Pilot. In 2018‑19, the Legislature approved budget‑related legislation establishing the San Mateo Health Plan Dental Integration Pilot, whereby San Mateo’s Medi‑Cal managed care plan would cover its beneficiaries’ dental services in addition to physical health services. The Governor’s proposal to end dental managed care does not affect the San Mateo dental integration pilot.
Assessment
Dental Managed Care Pilot Has Not Achieved Its Objectives. Dental managed care has faced a number of challenges over the course of its implementation, most notably related to low utilization of dental services by plan members. In 2018‑19, the last year for which data are available on DHCS’ website, utilization rates of dental services are around 15 percent lower in dental managed care compared to dental FFS. Preventive dental service utilization rates in dental managed care are even lower relative to dental FFS. Despite lower utilization, per capita Medi‑Cal spending is around 50 percent higher in dental managed care compared to dental FFS. Finally, in Los Angeles, where dental managed care is optional, a small percentage of Medi‑Cal enrollees have opted to enroll, with the vast majority electing to obtain their dental benefits through FFS. Given the lower utilization, higher costs, and low participation where it is voluntary, dental managed care does not appear to be fulfilling the pilot’s legislative intent of achieving savings while ensuring access and quality.
Recommendation
Use Budget Process to Learn More About the Potential Trade‑Offs of Transitioning to FFS. We have some outstanding questions related to the Governor’s proposal to end dental managed care. First, we have yet to see a detailed transition plan. Therefore, to ensure appropriate legislative oversight over the transition from dental managed care to FFS, we recommend using the budget process to ask DHCS to share a detailed transition plan, including what efforts are being made to prevent disruptions in services for current dental managed care enrollees. In addition, we recommend that the Legislature ask DHCS and the dental managed care plans to share if there has been further improvement in dental managed care plan performance over the last year.
Approve Governor’s Proposal Assuming No Clear Information on Improved Dental Managed Care Plan Performance. If information from DHCS and the dental managed care plans gathered during the budget process clearly shows that dental managed care is on track to achieve at least comparable outcomes with dental FFS in terms of access and cost‑effectiveness, the Legislature could consider deferring action for a limited period of time on a decision about the future of dental managed care in the pilot counties. This would give the Legislature additional time to assess dental managed care plan performance to determine whether the legislative intent of achieving savings while ensuring access and quality is being achieved. If no new information comes to light during the budget process that clearly shows comparability in outcomes between dental managed care and FFS, we recommend approval of the Governor’s proposal to end the dental managed care pilot, along with continued legislative oversight of the transition to FFS to ensure successful implementation.
Summary of Recommendations
|
Issue |
Governor’s Proposal |
LAO Recommendations |
|
Medi‑Cal pharmacy services |
Carve pharmacy services out of managed care and transition to fee‑for‑service. |
|
|
340B clinic supplemental payments |
$26 million in 2020‑21, $53 million ongoing to fund supplemental payments for clinics participating in the 340B program. |
|
|
Non‑Medi‑Cal prescription drug rebates |
Authorize DHCS to collect rebates on prescription drugs not paid for by Medi‑Cal. |
|
|
SNF rate reform |
Reauthorize SNF rate‑setting framework, with various changes to increase the role of quality in the rates. Also increase authority to collect delinquent QAF. |
|
|
County administration |
Provide a COLA for county administration. Permanently extend temporary resources for two positions related to oversight of county administration. Reinstate and build on county performance measurement programs. |
|
|
Medi‑Cal dental services |
End dental managed care pilots and transition all Medi‑Cal dental services to fee‑for‑service. |
|
|
DHCS = Department of Health Care Services; SNF = skilled nursing facility; QAF = quality assurance fee; and COLA = cost‑of‑living adjustment. |
||
